|
 |
 |

September / October 2008

Effective Use of Medication-Related Decision Support in CPOE
By Jane B. Metzger, BA; Emily Welebob, RN, MS;
Fran Turisco, BES, MBA; and David C. Classen, MD, MS
If the rollout of computerized physician order entry (CPOE) follows on the heels of other advanced clinical system applications with significant decision support, such as electronic medication administration (eMAR) or clinical documentation, a core team of nurses, physicians, and pharmacists has already learned about the responsibilities and work of applying decision support on a large scale. However, in many hospitals, CPOE is the first advanced clinical application, and clinical decision support (CDS) applied so broadly is new and uncharted territory. Taking full advantage of this new capability to improve medication safety requires mastering each of the areas discussed below.
Build the structure for accomplishing the work of applying clinical decision support.
The logic of clinical decision support tools in CPOE that can guide and critique ordering is eventually applied to every targeted type of physician order. Mindful of what is at stake, hospitals proceed cautiously and deliberately. By now, most hospitals have invested in new group and individual roles and responsibilities to address quality and patient safety overall, and that structure is charged with integrating CDS into the strategy and tactics for improving medication safety (Provonost et al. 2008). Accomplishing this requires clear accountability and new processes to cover some areas such as the work of setting up and testing CDS, as well as ongoing monitoring and updating.
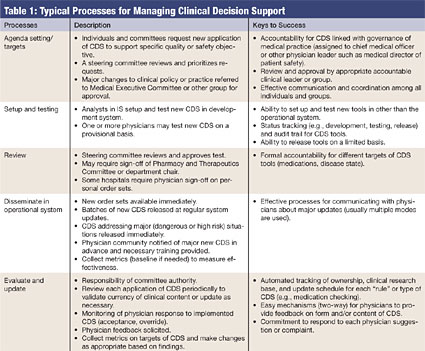
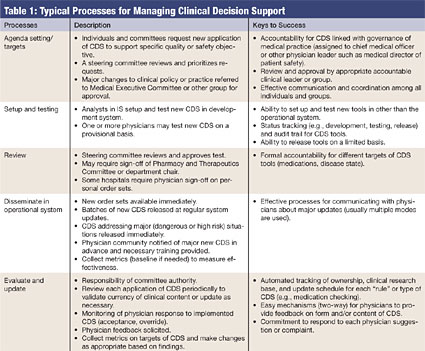
The major tasks of managing CDS tools are listed in Table 1 (pg. 18), along with recommendations and observations from many hospitals visited during development and testing of the evaluation tool and in other CPOE-related research (Metzger & Fortin, 2003; First Consulting Group, 2006). Although staff from the Information Systems Department (IS) — usually one or more physicians or nurse analysts who have mastered the CDS tools — play an important role, physician leaders (and to some extent pharmacists) with responsibility for patient safety own and lead this process.

|
 |
 |
 |


















|
 |