 |
 |
 |

March / April 2006

Six Sigma and Change Management
Reducing Hospital-Acquired Pressure Ulcers
By Senaida Garza, RN, BSN;

Veronica Okere, RN, CWOCN;

Jackson Igbinoba RN, BSN;

Kristi Novosad, RHIA; and Carolyn Pexton
Pressure ulcers or PrUs represent a serious problem for patients within the acute care setting, and a significant care management challenge for clinicians. Also known as bed sores, pressure ulcers have been classified by the Agency for Health Care Policy and Research (currently the Agency for Healthcare Research and Quality [AHRQ]) as "lesions caused by unrelieved pressure that results in damage to underlying tissue." Pressure ulcers particularly affect the elderly and patients with impaired mobility, and as the population ages, the incidence of PrUs is likely to increase.
In addition to the adverse impact on clinical quality and outcomes, the annual cost for treating nosocomial PrUs has been estimated between $2.2 and $3.6 billion. To mitigate the physical, psychological, financial, and compliance issues associated with this condition, it is important for hospitals to implement effective reduction and prevention strategies.
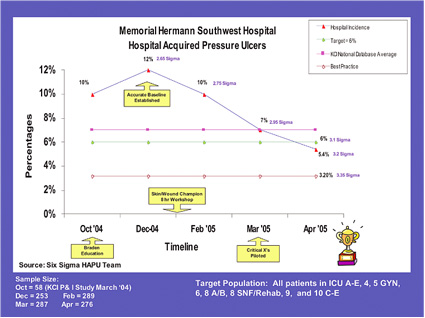
At Memorial Hermann Southwest Hospital (MHSW) in Houston, ensuring patient safety and quality are among the top priorities for improvement initiatives involving methods such as Lean Six Sigma and Work-Out. In 2004, the hospital noted a 12% incidence in hospital-acquired pressure ulcers, a rate that is above the 7% national average.
A multidisciplinary team at the hospital began a Six Sigma project in October 2004 targeting a 50% reduction in the incidence of hospital-acquired pressure ulcers within a 9-month period. They anticipated benefits from successfully completing this project would include the following:
- Improve customer satisfaction by providing best practice in skin and wound care.

- Avoid the risk of lawsuits.

- Avoid "fines" from regulatory agency (CMS) in SNF/LTAC units

- Reduce specialty bed rental cost by $125,000.

- Reduce length of stay associated with Stage III, IV, and "Unable to Stage" PrUs

- Reduce supply costs.
Define and Measure
The Six Sigma DMAIC process is built around five structured phases: Define, Measure, Analyze, Improve, and Control. With Six Sigma, the idea is to reduce defects or errors to a mere 3.4 per million opportunities and to statistically control key processes to minimize variability. Participants who go through the training and complete projects assume various levels of expertise as Green Belts, Black Belts, and Master Black Belts.

 |
|
Click here to view a larger version in a separate window.
|
As they began the initial Define phase of this Six Sigma training project, the team included three nurses: Cindy Garza as the Black Belt guiding the process, and two Green Belts. They expanded the size of the team once they realized they would also need additional skin and wound champions within the organization to change practice. A physician champion and a certified wound-ostomy-continence nurse (CWOCN) provided valuable input along the way.
In terms of scoping, the project would focus on all areas where pressure ulcer prevention and reduction should be a priority. Units considered outside the scope were the normal newborn nursery unit, emergency department (at least in the beginning), and labor and delivery. They defined a defect in this project as a patient with one or more hospital-acquired pressure ulcers.
The team began its work by gathering "VOC" or voice of the customer. They interviewed key personnel with a stake in reducing pressure ulcers. They also talked to some of the elderly volunteers who may have also been patients in the hospital. The interviews were designed to elicit perspectives on incidence rates, what steps should be taken, and what the current practices were that might contribute to pressure ulcers.
The VOC provided some surprising insights. Looking at a problem from a variety of angles instead of a single vantage point can be very beneficial. Patients and nurses from other areas of the hospital might see the issue in different ways, and specific concerns may surface. In this case, it turned out that the idea of changing practices would be a concern the team would need to address.
Understanding incidence rates and best practices from other hospitals can also furnish useful information during the Define phase. The team looked at national data and compared performance within their own multi-hospital system. Two of the other hospitals in their system had managed to reduce the rate of PrUs to between 4% and 6% of the inpatient population. Networking with other hospitals that had applied Six Sigma methodology to this issue also provided valuable guidance and advice.
Prior to this project, measurements from the hospital's skin team had indicated a 10% incidence rate for pressure ulcers. During the Measure phase, however, steps were taken to ensure the accuracy of the data collection process and measurement system analysis. The use of statistical tools such as gage R&R helped to correct inconsistencies and subsequently confirmed a higher rate of pressure ulcers at the hospital.
Once the tool and collection method had been validated, the skin and wound champions would go from room to room and gather the data. In order to actually change practice, it was important to involve the skin and wound champions in regular meetings. The chief nursing officer attended the initial meetings, and this motivated the skin wound champions to participate in the Six Sigma process.
An essential part of the initiative would be the use of the Braden Scale. This is a widely used rating tool that allows nurses and other clinicians to score a patient's risk for developing pressure ulcers. It is comprised of six subscales that measure functional capabilities: sensory perception, moisture, activity, mobility, nutrition, friction, and sheer. A lower Braden Scale Score indicates lower levels of functioning.
Before the project could move ahead, the team needed to make one rapid improvement. The WOCN had found a mistake — scoring criteria was missing from the bottom of the nursing record, but various interventions indicated what to do based on different scores. Nearly 500 nurses didn't have a scoring tool so they were essentially guessing at whether they were doing the right thing based on their experience and information at hand. The team quickly created a Braden tool with the print shop and trained nurses to use the scoring and intervention techniques.

 |
|
Click here to view a larger version in a separate window.
|
A Learning Process
The first step in collecting valid data would be to make sure the skin and wound champions would be able to correctly identify a wound on a patient's skin. All nurses provide assessments, but for the purpose of this project, additional expertise would be required. Fortunately, the hospital had hired a certified wound-ostomy-continence nurse (CWOCN) as an expert in wound management. She worked closely with the skin and wound champions to make sure they could accurately evaluate a patient's skin and identify any signs of pressure ulcers.
Lack of communication is a common barrier to improvement efforts in healthcare. Establishing ongoing communication and educating the nurses on Six Sigma would be key to the team's success. To promote buy-in, skin and wound champions needed to become familiar with the terminology and concepts. This would also convey the fact that they would ultimately assume ownership for the project and its outcome.
Creating an "elevator speech" helped to quickly convey the purpose of the project, and the use of Change Acceleration Process (CAP) tools helped to overcome any barriers between participants. Educational opportunities were available outside the hospital, helping nurses to learn more about the elements of skin wound management and best practices in the industry.
It is often hard to have nurses leave the bedside to attend meetings. This required coordination and advance notice so they could be relieved of patient care. It also meant getting buy-in from nursing management to cover scheduling and other adjustments.
As the project moved into the Analyze phase, the importance of prioritizing and concentrating on the most critical factors became very apparent. The team had developed a fishbone diagram to understand all the elements that might contribute to the overall outcome, such as personnel, materials, and the environment. Rather than trying to fix everything at once, statistical analysis helps to impartially focus the team's efforts on issues that will yield the greatest impact. Interestingly, nurses surfaced as a more pivotal group than physicians in terms of the critical input and process variables that drive hospital-acquired PrUs. The use of FMEA, or Failure Modes Effects Analysis, proved to be very helpful during the Analyze phase. Dividing the team into two meetings, they walked through all the steps from patient arrival to the moment the patient left the hospital, to determine how a patient might acquire a pressure ulcer.
Beginning with skin assessment and whether a pressure ulcer developed, the team learned through FMEA to examine and expand safeguards in place to catch opportunities for failure. This turned out to be an area needing improvement within their organization. The hospital routinely collected a great deal of data, but it wasn't really reported. The use of FMEA was an eye-opening experience and enabled prioritization of the hospital's efforts.
Using statistical tools such as regression analysis, data can be entered before a pilot begins to make sure the project is headed in the right direction. For instance, entering information about whether Braden scoring influenced the rate of hospital-acquired pressure ulcers produced a strong positive linear regression line. The diagram provides a compelling visual representation that demonstrates the importance of certain factors.
At the outset of this project, the suggestion was to create a wound management protocol or some standardization of orders to guide people on what to do. The statistical analysis, however, contradicted that idea, emphasizing improvements to be made in communication and assessment. This relates to the notion of culture change — the need for better dialogue with nurses and better documentation. Practice guidelines may tell nurses what to do, but they won't be ingrained without behavioral change and acceptance.
Monthly prevalence and incidence audits were performed based on the results of the analysis, providing a snapshot on every patient to determine the existence of pressure ulcers. This regular reporting established greater confidence and provided a solid foundation for introducing any new initiatives in wound management.
Solutions and Results
During the Improve phase, the team conducted an Action Work-Out to get everyone involved in designing solutions. The administrative team signed off on the process and the recommendations, giving the nurses the power to plan and proceed with three pilots.
Pilot A would involve weekly skin documentation audits. The team devised a tool based on chart review and decided this would be done every Tuesday. The skin and wound champions would note whether a skin assessment and Braden score had been done on admission of the patient, and on a daily basis. Additional elements were added later. After a successful 2-week pilot, the process moved to other units.
Pilot B involved nurse-to-nurse communication. The goal was to increase reporting between nurses on the patient's skin status, Braden score, and Braden score interventions. Some areas tape reports from shift to shift, so skin and wound champions would ask nurses not to erase reports before an audit could be performed. ICU implemented "Daily Interdisciplinary Rounds," in which bedside nursing involves pharmacists, Infection Control, and a case manager coming together to discuss a patient, and this provided the opportunity to talk about the Braden score or skin status and treatment.
Pilot B was also monitored for 2 weeks before taking it hospital-wide. The third pilot would be nurse-to-physician communication. The goal was to have physicians document the pressure ulcer so coders could pick it up, and the hospital would be reimbursed appropriately. This pilot was postponed based on input from the physician champion, who suggested waiting until nursing had completed their process changes, and then work with physician champions in writing actual skin and wound management protocols.
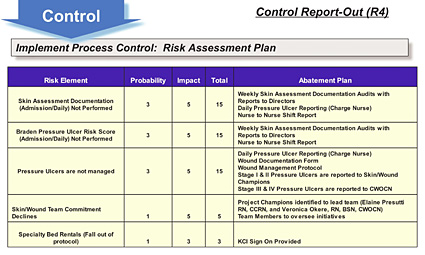
The improvements produced excellent results that were shared at report-outs attended by leadership and the skin wound champions. By the Control phase, the team had surpassed its goal of 6% of the inpatient population — a 50% reduction — and had achieved a rate of 5.4%. Recently, this has been further improved to 2.7%, which is considered best practice. In addition to increasing safety and quality of care, the financial benefits from the project include a $1.2 million cost savings within the first 6 months and expect a $2.4 million annualized cost savings, reducing annual rental of specialty bed units by $125,000 and avoiding the potential for costly lawsuits.
It is important to recognize and celebrate success with any improvement initiatives. Following the final report-out, the project team brought together several units, including ICU, skilled nursing, and rehab, and had an ice cream and cupcake party to celebrate their achievements in this critical area.
Beyond the specific results in reducing pressure ulcers, one of the best outcomes of the project was the development of a strong network among the nurses. They are now communicating and collaborating much more effectively, which ultimately translates to better care and coverage of individual patients.
To make sure progress is maintained, the skin audits and monitoring processes are continuing. An important aspect of the Control phase involves identifying someone to assume ownership and evaluate other critical factors or "X's" and how they will be addressed. Next steps involve reviewing the diagram and determining other stakeholders who should be involved in the process. For instance, patient care associates (PCA) or nurse associates will be starting a pilot project called the PCA skin saver. They will carry a notebook with a body diagram and will be taught how to identify red spots that could indicate a potential skin breakdown.
One of the co-developers of the Braden tool, Dr. Nancy Bergstrom, came to Southwest during Nursing Week and said PCAs can also be taught how to Braden a patient. Her presence at the hospital helped to validate the hard work the nurses are doing instilling Braden as a common practice. Dr. Bergstrom was very impressed with the hospital's skilled nursing unit, currently at 100% compliance for identifying patients at risk, with zero incidents of pressure ulcers for several months.
Prior to being certified as a Six Sigma Black Belt in October 2005, Cindy Garza served for 19 years as a nurse in roles such as ICU staff nurse and charge nurse, medical/surgical staff nurse, administrative coordinator for nursing administration, and coordinator for pain management and continuing nursing education. At Memorial Hermann Southwest Hospital in Houston, she works on healthcare improvement projects such as reducing hospital-acquired pressure ulcers and catheter-related bloodstream infections. Garza is currently working toward a master's degree in nursing at the University of Texas, Tyler.
Veronica Okere has been a nurse for more than 32 years and currently is a clinical educator for the Memorial Hermann healthcare system in Houston. She received her first training in Nigeria, followed by a bachelor's degree in biology and psychology from the University of Minnesota, and a bachelor of science in nursing from the University of Texas Health Science Center in Houston. She is also a graduate of the wound, ostomy, and continence specialty program at the University of Texas MD Anderson Cancer Center in Houston.
Jackson Igbinoba is a clinical manager and Six Sigma Green Belt at Memorial Hermann Southwest Hospital. He has been a nurse for 11 years and in his current role as a nurse manager for the past 8 years. He received the Memorial Hermann Southwest Nursing Clinical Excellence Award in 2001, the Houston Chronicle Salute to Nurses Award, as well as the Nurse Week Nursing Excellence Award for Mentoring, in 2004.
Kristi Novosad is director of health information management at Memorial Hermann Southwest Hospital and serves as the hospital and corporate team leader for the information management chapters of the JCAHO and CMS accreditation standards. She is a certified Six Sigma Green Belt and has recently completed a Six Sigma project on reducing catheter-related bloodstream infections in the intensive care unit; which reduced the rate by 50%. Current projects include surgical site infections and OR supply cost.
Carolyn Pexton has more than 20 years experience in communications and healthcare and is currently serving as the director of communications for Performance Solutions at GE Healthcare. In this role, she manages public relations, marketing communications, and organizational communications for GE's Performance Solutions group. She also works closely with customers to publicize their achievements through articles and speaking engagements. Pexton is a certified Six Sigma Green Belt and has presented and published on a variety of topics including Lean Six Sigma and change management within the healthcare industry. She can be reached at carolyn.pexton@med.ge.com.
References
Fisher, A. R., et al. (2004, March). Factors associated with pressure ulcers in adults in acute care hospitals. Advances in Skin & Wound Care.
Fleishman, A. (2005, January). Adult wound care — Management of pressure ulcers, For The Record. 17(1), 42.
Langemo, D., et al. (2003, October). Uncovering pressure ulcer incidence. Nursing Management.
Whittington, K. T., & Briones, R. (2004, November/December). National prevalence and incidence study: 6-year sequential acute care data. Advances in Skin & Wound Care.
|
 |
 |
 |


















|
 |



