PSQH Quick Poll 2024: Taking the Pulse of Infection Prevention Efforts
By Jay Kumar
As part of PSQH’s celebration of International Infection Prevention Week, we decided to reach out to our readers with a few questions to find out the state of infection prevention efforts.
The Quick Poll had a total of 146 respondents. Thanks to sponsors BioVigil and Inovalon.
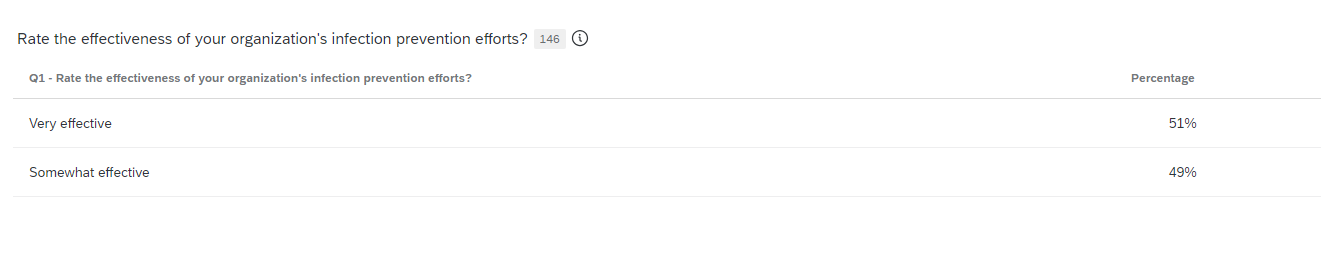
Infection prevention efforts
Asked to rate the infection prevention efforts of their organization, 51% of respondents said their program was very effective and 49% said their organization’s infection prevention was somewhat effective.
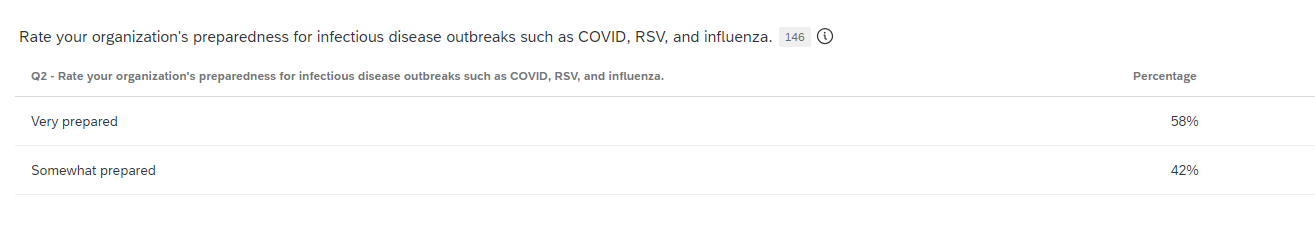
Organizational preparedness for infectious disease outbreaks
Flu season is here and COVID-19 remains a concern along with other viruses. From an organizational standpoint, a majority of respondents (58%) to the PSQH Quick Poll said they are very prepared for infectious disease outbreaks. Another 42% said they are somewhat prepared for future outbreaks.
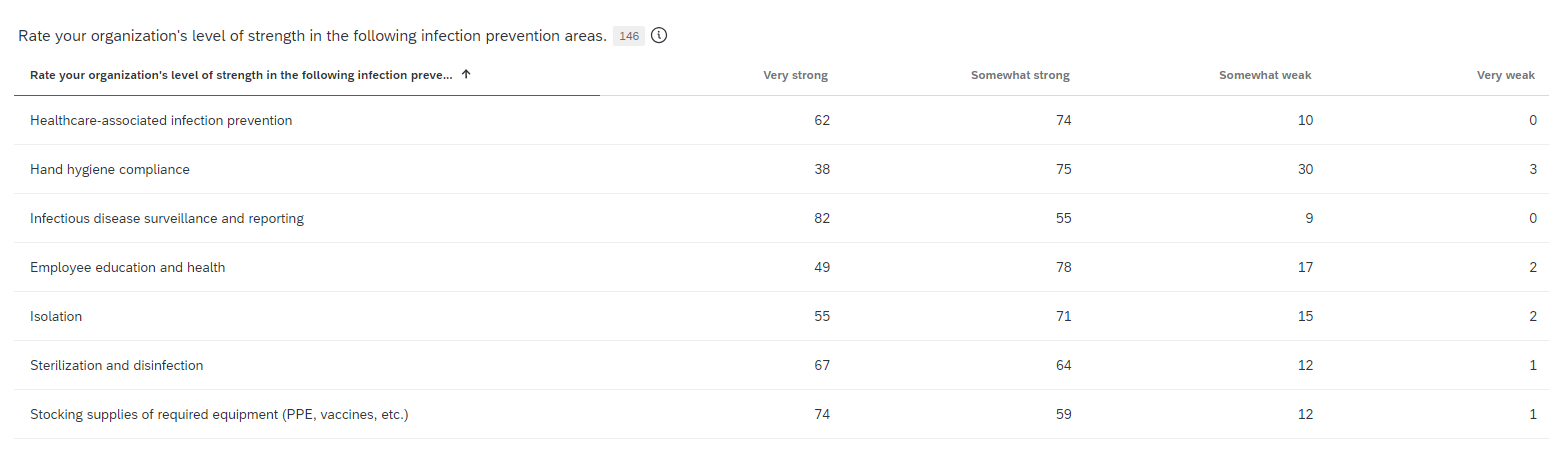
Strength in various infection prevention areas
We queried respondents on their perceived level of strength in various infection control areas. When it comes to healthcare-associated infection prevention, 43% of respondents say they are very strong, 51% say they’re somewhat strong, and 6.9% say they are somewhat weak. With hand hygiene compliance, 26% of respondents say they are very strong, 51.4% say they are somewhat strong, 20.6% consider themselves somewhat weak, and 2.5% say they are very weak.
Infectious disease surveillance and reporting was the strongest area, with 56.2% of respondents saying they were very strong, 37.7% saying they were somewhat strong, and 6.2% saying they were somewhat weak.
In the area of employee education and health, 33.6% say they are very strong, 53.4% say they are somewhat strong, 11.6% say they are somewhat weak, and 1.4% say they are very weak. With regards to isolation, 37.7% say they are very strong, 48.6% say they are somewhat strong, 10.3% say they are somewhat weak, and 1.4% say they are very weak. In sterilization and disinfection, 43.8% say they are very strong, 40% say they are somewhat strong, 8.2% say they are somewhat weak, and 0.7% say they are very weak.
Asked about stocking supplies of required equipment (PPE, vaccines, etc.), 50.7% say they were very strong, 40.4% say they were somewhat strong, 8.2% say they were somewhat weak, and 0.7% say they are very weak.
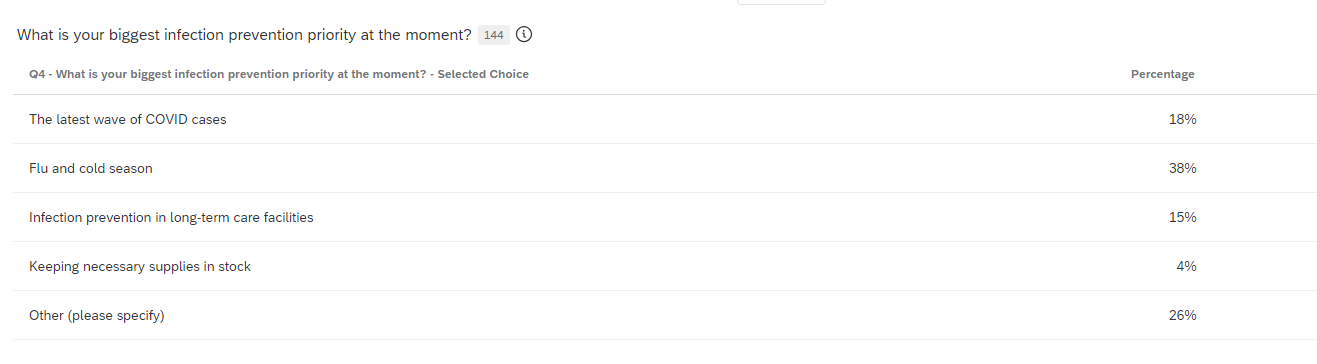
Biggest priority
Asked about their biggest infection prevention priority at the moment, 38% of respondents say it was flu and cold season. Another 18% say the new wave of COVID-19 cases, 15% say infection prevention in long-term care facilities, and 4% say keeping necessary supplies in stock. Other write-in responses included: M-pox management, impact of staffing challenges, healthcare-associated infections, tuberculosis, scabies, carbapenem-resistant organisms (CRO), CAUTI and CLABSI prevention, healthcare workers’ understanding of infection prevention, leaders and associates being receptive to infection prevention education or recommendations, high-level disinfection and sterilization, adjusting for surveillance for all inpatients to population-based, enforcing basic infection prevention measures and leadership buy-in to hold staff accountable to practices, maintaining communication with employees about potential outbreaks, employee handwashing, education and competencies of staff, surgical site infections, ordering and receiving current influenza and COVID vaccines, emerging pathogens (C. auris, measles, etc.), and meeting all reporting requirements.
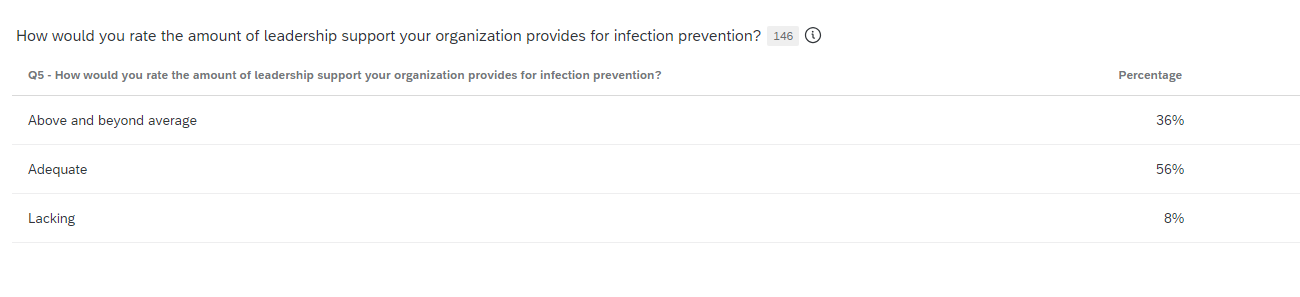
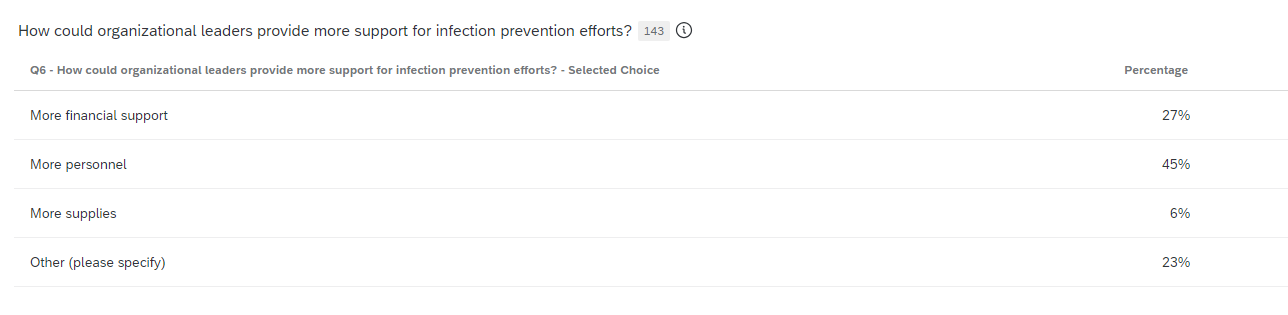
Leadership support for infection prevention
Asked to rate the amount of leadership support for infection prevention, 36% of respondents say it was above and beyond average, 56% say it was adequate, and 8% say it was lacking. When respondents were asked how leaders could show more support, 45% say more personnel, 27% say increased financial support, and 6% say more supplies. Other write-in responses include more engaging activities for frontline personnel, react to new HAI, more training for screening, following through with Infection Control’s recommendations, supporting infection preventionists as subject matter experts and following guidelines, increased education and communication, a seat at the table, consequences for those not following intentionally, increase personnel and pay rate, better engagement in process, better oversight and accountability, education for leaders on the importance of infection control and prevention and the needed focus and support for the program/department, prioritize resources for education of staff, keeping staff abreast of latest infection prevention data, more C-suite presence in the effort to keep moving toward zero, more awareness and engagement, walking rounds each shift to view and address gaps in practice, and staff recognition.