Using Six Sigma to Improve Patient Safety in the Perioperative Process
July/August 2013
![]()
Using Six Sigma to Improve Patient Safety in the Perioperative Process
Background
In this project, the Six Sigma methodology was utilized to improve patient safety and compliance to the Time Out protocol and certain Surgical Care Improvement Project (SCIP) measures. The project took place in the perioperative service at Huntington Hospital, in Huntington, New York. Six Sigma is an improvement science that utilizes a structured approach known as DMAIC (Define, Measure, Analyze, Improve, and Control) and a series of improvement tools in order to identify sources of variation and to develop improvement strategies that would lead to the reduction of opportunities for defects and variation in a process or system.
Throughout the surgical experience, patient safety is a critical quality aspect of a hospital’s performance. Appropriate completion of the preoperative assessment of the patient, known as a Time Out protocol, is often the main mechanism utilized in a surgical environment to ensure patient safety. The protocol is a process for reviewing and verifying key components in patient identification prior to the start of incision, and is the most valuable process for preventing “Never Events” such as wrong-person, wrong-site, and wrong-procedure errors.
To measure the quality of hospital care throughout a patient’s surgical experience, the National Quality Forum (NQF) provides SCIP measures, which are evidence-based practices bundled together to prevent intra-operative complications and reduce postoperative surgical site infections. Hospitals are expected to conform to the SCIP measures to provide high quality care and receive appropriate financial reimbursements from Centers for Medicare and Medicaid Services (CMS). Five of the SCIP core measures can be accomplished prior to the start of any procedure or surgery. Inclusion of these issues during the surgical Time Out process can ensure compliance and thus help prevent complications and infections.
This project uncovered that the traditional paradigm of patient safety in perioperative service encompasses two separate processes, one of which involves the wrong-site surgery Time Out protocol and a second component that involves the SCIP measures.
In order to provide a more robust approach to patient safety in perioperative services, the team viewed the patient through the lens of rolled throughput yield, which is a concept that approaches patient safety as one cumulative process, viewing the Time Out protocol and SCIP measures as one consistent process. The performance of processes and steps are interrelated. Through the lens of rolled throughput, a patient should pass through the cumulative steps of the total safety process free of defects or issues.
Setting
Huntington Hospital is a community-based hospital in the North Shore–LIJ Health System located on Long Island, New York. Within the perioperative department at Huntington Hospital, a majority of the surgeons are in private practices and have been given privileges to perform surgical procedures at the hospital.
Scope of the Project
The core team consisted of three frontline employees from nursing, nursing management, and quality management, all of whom acted as Six Sigma Greenbelts on the core team. Additional frontline employees, surgeons, and anesthesia also participated in the project in the role of extended team members, in which they provided resource support to the project.
The first step in the Six Sigma deployment was the development of a project charter, which outlined the problem statement, goal statement, business case, and scope of the project. The project included all adult surgical cases and five of the SCIP core measures, including: foley insertion, antibiotic time, antibiotic selection, beta blocker, and normothermia.
Define Phase
The development of a high-level process map (Figure 1) enabled the graphical depiction of the safety process; this process map helped the team understand the patient safety process and the extent of the issue involving compliance to the Time Out protocol within the perioperative service line.
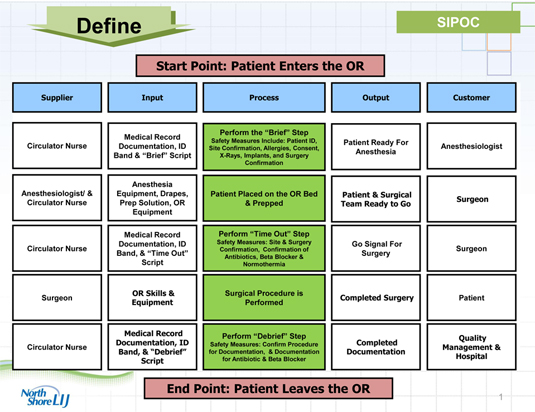
Figure 1. High Level Process Map (click here to view a larger version in a separate window)
Notes:
Supplier: The person or organization who provides the inputs to your process.
Input: The materials, resources, and data required to execute your process.
Process: The series of steps or activities that use one or more kinds of INPUTs and changes them to an OUTPUT that is of value to the CUSTOMER.
Output: The tangible products or services that result from the process.
Customer: The person or organization that receives the outputs of the process.
The objective of this Six Sigma deployment was to improve compliance to the safety process and to introduce a robust approach to patient safety and quality. Based on findings from the Define phase, two metrics were defined to measure the baseline performance of this process and develop the goals of the project. The first metric was identified to be compliance to the Time Out protocol: the completion of the applicable safety requirements and SCIP core measures in proper sequence and at the proper time of the safety protocol. The second metric was the cumulative total time to complete the Time Out protocol during the surgical experience (in minutes) including the brief, Time Out, and debrief safety stops. Note that the second measure was included in the project since the voice of the customer (surgeon feedback) identified that main drawbacks to the safety protocol were that it was too cumbersome and took too long to complete.
Measure Phase
The Measure phase established baseline performance for the organization with two performance metrics. Data was collected through two mechanisms: an observational study and a retrospective extraction of data from patient charts. The data collection tools were validated for accuracy, repeatability, and reproducibility prior to being fully rolled out to the perioperative service organization. The data collection was performed on 88 cases.
Baseline measurements indicated that average compliance to the safety process was 93.15%, with a minimum compliance level of 78.26%. The preliminary analysis also indicated that amount of variation in the process (assessed by the standard deviation) was 6.24%. The initial capability of the process found a Defects Per Million Opportunities (DPMO) of 784,091 with a sigma score of 0.71. This performance meant that with the original safety process, only 79% of the surgical cases were provided with the complete (all requirements) safety protocol.
The recommended performance goal was to reduce the standard deviation to 0.50% and reduce the DPMO by 85%, which in turn would raise the sigma score to approximately 2.69. In addition, the target compliance level was set at 100%, with a lower specification limit (LSL) of 97.5%, the minimal level required to allow the organization to achieve top decile performance in safety during a surgical procedure. The LSL is a lower limit below which the process performance is deemed unacceptable or a “defect.” By achieving the minimal compliance level needed to achieve top decile performance in terms of safety, quality, and SCIP core measures, the hospital will be able to maximize its financial reimbursement from CMS and minimize potential financial penalties related to surgical quality care.
The preliminary analysis also found that the average time to complete the safety process was 3.10 minutes; variation in the process (assessed by the standard deviation) was 0.56 minutes (or 34 seconds). The initial capability of the process found a DPMO of 34,091 with a sigma score of 3.32. The preliminary analysis found if the safety process is done properly, it does not take a long time to complete. The safety process was found to take longer in the cases where team members were not present to start the process or if the surgical team had to “redo” the process because the team failed to complete a specific safety requirement. The recommended performance goal was to reduce the standard deviation to 0.20 minutes (12 seconds), with a target average value of 3.10 minutes, and reduce the DPMO by 65%, which in turn would raise the sigma score to 3.76.
Analyze Phase
The Analyze phase evaluated all of the potential factors (Xs) that impact the performance and identified those few vital Xs that have the most significant impact on performance. By identifying the vital Xs, improvement strategies can focus on the factors that are the most critical to the process. The data collected in the Measure phase were analyzed in order to identify sources of variation in the process.
The first tool utilized in the Analyze phase was a fishbone diagram, which is a cause and effect display to identify potential factors that impact the “compliance to safety” outcome (Figure 2). It provides visual comprehension of the potential root causes of the issue and how they fit into the process.
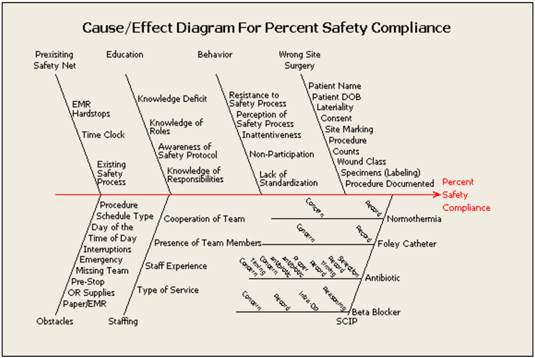
Figure 2. Cause and Effect Fishbone Diagram(click here to view a larger version in a separate window)
The second tool utilized was Failure Modes and Effects Analysis (FMEA). This tool identifies potential and actual points of failure in a process as well as potential corrective actions. More specifically, each failure mode is assessed and rated in terms of three criteria—severity, occurrence, and detection—which are rated on a scale of 1 to 10. For each failure mode, a risk priority number (RPN) is calculated by multiplying the severity by the occurrence by the detectability. For this project, any failure mode with an RPN greater than 150 was identified as critical and highlighted in red (Figure 3). The FMEA identified 24 items with an RPN greater than 150.
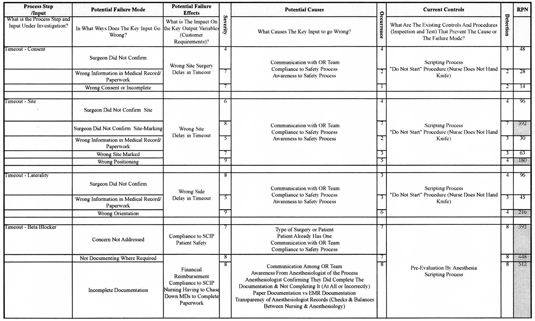
Figure 3. Failure Modes and Effects Analysis (FMEA)(click here to view a larger version in a separate window)
Notes:
Failure Mode: The manner in which a specific process fails.
Cause: A condition that produces a failure mode.
Failure Effect: Impact on customer requirements if failure mode is not prevented.
RPN: Risk Priority Number, which is computed by multiplying the “severity” by the “occurrence” by the “detectability.”
RPNs highlighted in red: Process steps that resulted with an RPN greater than 150.
The final tool was hypothesis testing, which utilizes graphical tools and statistics to identify the probability that a stated hypothesis is true. In summary, a series of hypothesis tests were examined by computing a p-value, which is the probability value or observed significance. The use of the p-value provided the ability to decipher which factors (Xs) were vital.
These analysis tools were used to identify factors that had the most significant influence on the performance of the process. The analysis identified that there was no standardization of the original safety process; despite having a script to use during the case, the surgical team could complete safety steps in a different order than originally designed, including or excluding any safety requirements they deemed appropriate. In addition, there was insufficient verifying communication between team members during the safety process; a team member could state the completion of a requirement, but other team members would not verify that statement. More specifically, one key safety requirement for patients taking a beta blocker was typically skipped or incorrectly addressed by the surgical team at the time of the procedure.
In addition, the analysis identified the presence of the surgeon at the start of the safety process to be critical. On many occasions, the surgeon arrived late, which delayed the safety process and impacted how the staff perceived the process. In addition, after surgeons arrived to start the safety process, it was often difficult to keep them focused during the times that they were not active; this in turn made it more difficult for the nursing or anesthesia staff to communicate with them or gain their attention during the safety process.
The Analyze phase also found that the process was strongly influenced by the documentation of safety measures that were being completed by both the nursing and anesthesia staffs. On many occasions, the surgical teams provided incomplete or inaccurate documentation.
A final critical issue identified from the Analysis revolved around communication that occurred between team members throughout the case. Team members had difficulty communicating with each other for several reasons, such as team members who were unavailable because they were prepping the patient, talking on the phone, working on documentation, or had left the operating room for a prolonged period of time.
Improve Phase
The following vital Xs (elements) were identified for improvement:
- Standardization of the process flow
- Acceptance and perception of the safety process by the perioperative team members
- Presence of the surgeon to start the safety process
- Documentation related to the safety process
- Inconsistent communication throughout the surgical case
The next step was to design a specific set of improvement strategies to impact these vital elements.
Some of the improvement strategies were considered to be a “quick win,” in that they could be implemented quickly with immediate impact. One such strategy was to implement a “good catch” form for perioperative team members to use for reporting wrong-site surgery “near misses,” which tend to occur and are often unreported. Perioperative staff members were encouraged to complete a good-catch form whenever a near miss occurred and submit it to the through a drop box. This solution provided the perioperative service line with the means to identify, document, and report these incidences.
Another strategy involved the use of a beta blocker sticker to identify last dose taken, which is placed on the patient’s chart during intake assessment in the Ambulatory Services Unit (ASU), in order to provide a visual reminder (similar to a kanban signal) for the surgical team that the patient is on a beta blocker and that this factor is a safety concern that the team must address during the safety protocol.
Another improvement strategy used a preprocedure checklist as a communication tool between the ASU, perioperative holding room, and circulating nursing staffs. This checklist covers safety requirements that should only need to be addressed at one process step between ASU and the operating room, not repetitively at each process step. The checklist is completed as the patient moves through the process and helps improve the handoff communication between the staff members, reduce redundancy in the process, and provides a mechanism to document the completion of the safety requirements.
A final improvement strategy involved a SCIP checklist to be completed by the anesthesiologist. The Analyze phase found that poor compliance with SCIP documentation was due to the complex forms from the original safety process, which made it more cumbersome and difficult for the team to complete. The checklist contained checkboxes for each of the following SCIP quality measures: antibiotic selection, antibiotic administration, beta blocker, and normothermia. In addition, at the conclusion of the surgical case, the anesthesiologist hands the SCIP checklist to the circulating nurse, who verifies that the checklist is complete.
Two other improvement strategies required more time to develop and a series of pilot tests prior to full implementation into the perioperative service line. One of these involved eliminating non-critical steps requirements and maximizing value-added requirements, which reduced the process flow from 44 steps to 28 steps. In addition, we implemented a perioperative safety checklist for the new safety process, which also includes the “quick win” strategies already implemented into the process flow. The checklist and safety process were designed to improve standardization of the safety process, communication between the team members, accountability of completing the safety requirements, redundancy of the safety process, and acceptance and perception of the safety process.
We also implemented a paging system to help improve the on-time presence of the surgeon to start the safety process. The use of “coaster” pagers (similar to those used in the restaurant industry) was built into the reflowed safety process; each operating room is assigned a specific pager, and each pager has a designated phone number that activates the pager and communicates with the surgeon. Surgeons are given the pager when they come to mark the site and sign the consent in the holding room. They must return to the perioperative suite within five minutes when the pager goes off, as the patient is being moved into the operating room.
Both of these strategies were tested by running two pilot tests with different environmental conditions. Pilot 1 involved testing these strategies in two operating rooms with a controlled set of surgical service lines, nursing staff, and anesthesia staff. Pilot 2 included the original constraints of Pilot 1 but expanded the number of rooms from two to four, which, increased the number of surgical service lines and included all anesthesia staff. The pilot tests were utilized not only to test the improvement strategies but also to refine the strategies in order to obtain the optimal design for each strategy.
Control Phase
In this phase of the Six Sigma structure, the team was disbanded, and the process owners (nursing manager and quality coordinator from core team), who had been participating in the project since its inception, took ownership over the project in order to insure that the improvement strategies were not only implemented, but sustained over time. The process owners and Black Belt member utilized statistical process control (SPC) and a control plan to monitor the improvement strategies and vital Xs, measure improvements in the metrics, and ensure that the process is sustained over time. In addition, the team sponsor, nursing and physician staffs, and steering committee were updated by the process owners on a monthly basis through the use of constant data tracking.
Results
After the improvement strategies were implemented, data was collected and analyzed to highlight the postimprovement success of the process. Data was collected for 73 cases. The strategies resulted in improving process compliance to an average of 98.30% (from 93.15%) while reducing the standard deviation from 6.24% to 3.70%; this improved performance helped to reduce the DPMO by 82% (from 784,091 to 136,987), and increase the sigma score from 0.71 to 2.59. For this measure, the yield, which represents the percentage of the process that is acceptable to the customer, was raised from 22% to 86.50%, which means that 86.50% of the surgical cases performed can meet the LSL of 97.5%.
The improvement strategies were also able to reduce the variation related to completing the safety process to between 3 and 4 minutes. The average time to complete the safety process remained steady at 3.10 minutes (as desired) but the standard deviation was reduced from 0.56 minutes (34 seconds) to 0.17 minutes (10 seconds), both of which helped to reduce the DPMO from 34,091to 0; in turn, the sigma score was increased from 3.32 to 6.0. As a result, the yield for this measure was raised from 96.40% to 100%.
Discussion
This Six Sigma deployment provided the organization with a detailed analysis of the patient safety process within the perioperative service line. The Six Sigma methodology is a data-driven improvement science that utilizes the voice of the customer(s), data, statistical analysis, and other improvement science tools to identify the factors that are the most critical to the quality improvement for a process. The methodology stresses accountability throughout the project and constant evaluation of the process, which helps foster sustainability.
The frontline staff, surgeons, and anesthesiologists in the hospital were critical to this project during execution, design of improvement strategies, and holding the gains. Throughout the project, the team faced varying degrees of resistance from stakeholders in the organization, which it overcame by actively involving the frontline employees, surgeons, and anesthesiologists throughout the project and also maintaining constant communication with the stakeholders. The team regularly presented the progress of the project to many different venues and posted awareness flyers (Figure 4) throughout the perioperative suite to provide consistent updates about the project.
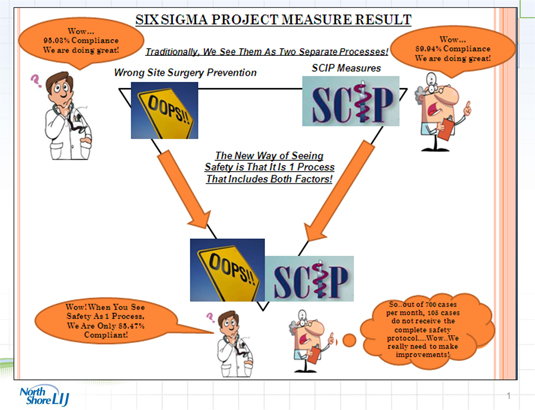
Figure 4. Measure Phase Awareness Flyer(click here to view a larger version in a separate window)
Continuous involvement and buy-in from the frontline staff, surgeons, and anesthesiologists helped design and implement the improvement strategies as well as establish a high level of engagement, which led to long-term sustainability. The Six Sigma methodology not only provided the organization and teams with the ability to implement improvement strategies into their process, but also gain the acceptance and support from the frontline employees and organizational leadership, all of which helped to drive process excellence and sustainability.
Nancy Riebling is the director of improvement sciences and a Master Black Belt for the North Shore-LIJ Health System. She holds master’s degrees in clinical chemistry and pharmacology and is certified as a Six Sigma Master Blackbelt. She may be contacted at nrieblin@nshs.edu.
Corazon Paraso is a quality and performance improvement manager at Huntington Hospital. She is a registered nurse and holds a master’s degree in Family Health Practitioner and is certified as a nurse executive and a critical care nurse. She may be contacted at cparaso@hunthosp.org.
Gina Lehmann is an assistant nurse manager in the perioperative department at Huntington Hospital. She is a registered pediatric nurse and a certified nurse operating room (CNOR). She may be contacted at glehmann@hunthosp.org.
Maria Yule is an operating staff nurse in the perioperative department at Huntington Hospital and is a certified nurse operating room (CNOR). She may be contacted at mayule@hunthosp.org.
About the North-Shore LIJ Health System
The North-Shore LIJ health system, headquartered in Great Neck, New York, encompasses five tertiary hospitals, seven community hospitals, two specialty care hospitals, one affiliate hospital, the Feinstein Institute for Medical Research, the Hofstra North Shore-LIJ School of Medicine, a network of rehabilitation and skill nursing facilities, a hospice network, a home care network, and a series of care centers that offer a wide range of outpatient services.
