The Patient’s Journey Through the Health System
By Cristina Vaz de Almeida, PhD
Although the concept of “service experience” was defined as “a subjective state of consciousness with a variety of symbolic meanings, hedonic responses and aesthetic criteria,” the concept now represents the human experience (Holbrook & Hirschman, 1982). In a broader concept, the patient experience integrates the sum of all interactions of patients, families, and care partners with the healthcare workforce, driven by cultures that support a healthcare ecosystem across the care continuum within communities (Wolf et al., 2014). This experience extends to all health organizations, whether primary care, hospital, private, or public organizations.
If health literacy promotes good system navigability in the dimensions of access, understanding, and use of health services and information (Sørensen et al., 2012), it is then necessary to list the problems, difficulties, required changes, and consequent improvements to make in a patient’s navigation through the complex health system.
Some of the points listed in health units’ user satisfaction questionnaires (Ferreira et al., 2017) reveal that patients complain about usually waiting a long time for their consultation. If they are in a private health organization, it may happen that patients are jumping from room to room, as if they were in a board game. Whether by phone, virtually, or in person, patients must give explanations to several people until they reach a healthcare professional. And when they are with the professional, usually the focus is on the current problem and not on the entirety of the patient’s well-being. Then the patient takes the reverse route, to either pay or get results … and the path unfolds in multiple stops.
Specific configurations and design elements may differ throughout the service continuum, but the objectives of safety, efficiency, satisfaction, and high-quality service remain constant. Therefore, the first step must be to listen to the patient and integrate them, at minimum, in the preparatory processes of reflection on change.
This change, whether in the area of human interactions, in processes and flows, or in physical characteristics (spaces/environments) should revolve around the perceived satisfaction of the patient, because it is they who will essentially use the services. However, pleasant spaces, simplified and standardized flows, and kind, assertive, clear, and positive people benefit everyone, including health professionals (Vaz de Almeida, 2016, 2019; Vaz de Almeida & Belim, 2021a, 2021b). Regarding investment in spaces for people with dementia, for example, Hopkins and colleagues (2017) showed that there is some evidence to suggest that residents with dementia in nursing homes sleep better when exposed to high levels of blue light.
Figure 1. The Service Experience
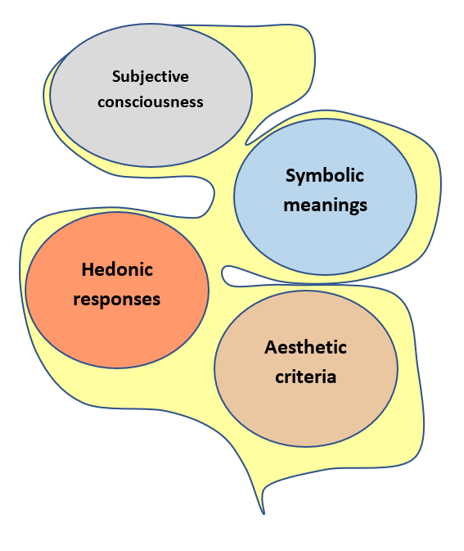
| Source: Based on Holbrook & Hirschman (1982). |
The patient is rational and emotional, so all their surroundings need to be integrated according to the patient’s sensory organs. Thus, it is important to see the healthcare journey through the patient’s eyes: their observations, emotions, and feelings; the usual route they take for services (outpatient clinic, urgent care, hospitalization, specialty care, etc.); the sensory qualities of each space and the equipment available for use. It is this sensory walk that allows the work of cognition with emotion (Damásio, 2020) and that allows an organization to provide a unique, satisfying, and memorable experience for the patient (Figure 1).
If we take into account the Weick model (1979) and its adaptation of the theory of sociocultural evolution (description of the processes by which people adapt to changes in their social and cultural relations to survive), we can observe the three phases that delimit the communication process such as regulation, selection, and retention (Kreps, 2009). Retention processes are essential in taking into account the patient’s feelings and emotions, and are used to preserve what was learned in the processes of regulation and selection, creating a set of experiences about what resulted and did not result. This critical analysis guides future research and selection within healthcare (Kreps, 2009).
Ike et al. (2019) focus on the use of the arts as a new way to boost engagement and promote health communication and health literacy. Engaging with the arts allows health professionals to improve their clinical competence, promote well-being, and prevent burnout.
Also, according to Global Guide: City Friendly to the Elderly (World Health Organization, 2008), “the interpersonal dimension of communication is very important, and it should be emphasized that the best way to be informed is to remain active and involved in the community.”
If we understand that one of the “root” problems is that many patients lack a perfect understanding of how to follow up on the instructions given by health professionals, we can understand what is happening in the mind of a person with low health literacy.
If, as Damásio (2020) states, the representations of images and objects of the external world provoke a certain image in the mind that may or may not be perceived, we understand that when there is no such representation, no image is recorded or understood. When patients hear technical jargon that they do not understand, there is no representation of image and correct information in their mind. They either do not understand or mistranslate what has been transmitted to them.
We know (Espanha et al., 2016) that vulnerable patients with low health literacy need an increased effort from health systems and professionals to achieve a more positive and effective experience when navigating the health system. These patients are in need of enlightening information to understand their health, deal with risk factors, and recognize the importance of social determinants. Therefore, it is necessary to create specific strategies for each of these patient profiles throughout their life cycle (see Table 1).
Table 1. List of Profiles With Low Health Literacy and Difficulty in Understanding Technical Health Instructions
| 1. Elderly
2. People with low levels of education 3. People with prolonged illnesses 4. People with a perception of “bad” health 5. People who have required primary healthcare six or more times in the last year 6. People who have chronic illness 7. People who have not learned to read or write 8. Groups of migrants 9. Long-term unemployed 10. People who do not follow health instructions due to cultural beliefs 11. People who have no access or low access to preventive screenings |
In this constant challenge for organizations, they need to understand the experience of their patients, not only at singular points of contact but throughout the patient’s journey.
Experiencing directly through the eyes of patients is one of the ways to identify areas for improvement and create new value. See Table 2 for some questions to ask the patient to improve your understanding of their experience:
Table 2. Questions to Assess the Patient’s Journey
| 1. What is your perspective?
2. How do you feel? 3. What are your experiences? 4. What are your fears? 5. In what situations do these fears occur (i.e., at what point of navigability in the system and in the hospital or health unit?) 6. Who are the facilitators of this journey? 7. Whom do you really trust? 8. What makes you move forward? 9. What kind of solutions do you appreciate to reduce tension and stress? 10. Where and when should you have access to facilitators? |
Using these patient responses, it is possible to solve the problem through small steps that lead to an improvement in the patient’s journey. See Table 3 for some areas you can invest in to improve the patient experience.
Table 3. Investing in the System to Improve the Patient Journey
| Consider improving the patient experience by investing in the following areas:
· Integrating new rest/well-being spaces (e.g., in facilities for people with dementia) · Simplifying forms · Incorporating calming sensory elements (e.g., smells, light, colors, etc.) · Encouraging social and more humanized conversation |
It is necessary to create teams and working groups to evaluate patients’ journey both in the health organization and in the related social organizations and community structures that interact with the healthcare system. By doing so, we can recover a value that all patients seek: quality and perceived satisfaction in the health system that leads to better outcomes and an increase in the health literacy of organizations and society as a whole.
Cristina Vaz de Almeida, PhD, is director of postgraduate health literacy at ISPA in Portugal.
References
Damásio, A. (2020). Feeling & Knowing – Making Minds Conscious. Temas e Debates.
Espanha, R., Ávila, P., & Mendes, R. M. (2016). Literacia em saúde em Portugal [Health literacy in Portugal]. Calouste Gulbenkian Foundation.
Ferreira, P. L., Raposo, V. M., & Pisco, L. (2017). A voz dos utilizadores dos cuidados de saúde primários da região de Lisboa e Vale do Tejo [The voice of primary health care users in the Lisbon and Tagus Valley region], Portugal. Ciência & Saúde Coletiva, 22(3), 747–758. https://doi.org/10.1590/1413-81232017223.33252016
Holbrook, M. B., & Hirschman, E. C. (1982). The experiential aspects of consumption: Consumer fantasies, feelings, and fun. Journal of Consumer Research, 9(2), 132. https://doi.org/10.1086/208906
Hopkins, S., Morgan, P. L., Schlangen, L. J. M., Williams, P., Skene, D. J., & Middleton, B. (2017). Blue-enriched lighting for older people living in care homes: Effect on activity, actigraphic sleep, mood and alertness. Current Alzheimer Research, 14(10), 1053–1062. https://doi.org/10.2174/1567205014666170608091119
Ike, J. D., Postlethwait, R., & Parker, R. (2019). Nurturing context: TRACE, the arts, medical practice, and health literacy. Information Services & Use, 39, 93–104. https://doi.org/10.3233/ISU-180040
Kreps, G. L. (2009). Applying Weick’s model of organizing to health care and health promotion: Highlighting the central role of health communication. Patient Education & Counseling, 74(3), 347–355. https://doi.org/10.1016/j.pec.2008.12.002
Sørensen, K., Van den Broucke, S., Fullam, J., Doyle, G., Pelikan, J., Slonska, Z., & Brand, H. (2012). Health Literacy and public health: A systematic review and integration of definitions and models. BMC Public health, 12(80,) 1-13.
Vaz de Almeida, C. (2016). Literacia em saúde: Os caminhos para uma maior capacitação dos profissionais de saúde [Health literacy: The paths to greater training of health professionals]. Congress of the Scientific Association of Nurses (ACE). Enformação Magazine, Supplement (July 2016), 8–15. https://www.acenfermeiros.pt//files/upload/revistas/suplemento-congace.pdf
Vaz de Almeida, C. (2019). Modelo de comunicação em saúde – ACP [Health communication model – ACP]. Enformação Magazine, 10, 20–22. https://issuu.com/ace-enfermeiros/docs/10__revista_ace.pdf_1
Vaz de Almeida, C., & Belim, C. (2021a). Health professionals’ communication competences as a light on the patient pathway: The Assertiveness, Clarity, and Positivity (ACP) model. International Journal of Applied Research on Public Health Management, 6(1), 14–29. https://doi.org/10.4018/IJARPHM.2021010102
Vaz de Almeida, C., & Belim, C. (2021b). Health professionals’ communication competences decide patients’ health: Proposal of a communication model. In A. Tkalac Verčič, R. Tench, & S. Einwiller (Eds.), Joy: Using strategic communication to improve well-being and organizational success, Vol. 5 (Chapter 12). Emerald Publishing. https://books.emeraldinsight.com/page/detail/Joy/?k=9781800432413
Weick, K. E. (1979). The social psychology of organizing. Addison-Wesley.
Wolf, J. A., Niederhauser, V., Marshburn, D., & LaVela, S. L. (2014). Defining patient experience. Patient Experience Journal, 1(1).
https://pxjournal.org/journal/vol1/iss1/3
World Health Organization. (2008). Guia global: Cidade amiga do idoso [Global guide: City friendly to the elderly]. Organização Mundial da Saúde. https://www.who.int/ageing/GuiaAFCPortuguese.pdf
