The Cooperative High Reliability Organization: Approaching a Zero-Defect Culture
It is then worth noting that the preventable complication rate is 3.67 times higher in the uncovered cohort (i.e., cohort 3) than in the covered cohort (i.e., cohort 2). The gap between the 2.66 times longer delay in the task and the 3.67 times higher complication rate implies an acceleration of the preventable complication rate is associated with the delay.
Discussion
The alerts put in place were for micro-targeting tasks at risk of failure in antibiotic stewardship. Increased alerts in pneumonia over time showed the dynamic nature of these alerts relative to just clinical triggers (e.g., labs, vital signs) since these tasks were being missed more often both relatively and absolutely as the study progressed, even while pneumonia cases were decreasing. Pneumonia cases declined during the duration of the study (i.e., from 178 in February to 128 in May, as we would expect with the end of flu season), but there was an unexpected increase in the tasks at risk of failure identified by the scoring model, leading to not just a relative increase in alerting (from 20% to 27%), but also an absolute increase (from 35 alerts in month three to 47 in month four).
This indicated the size of the Swiss Cheese Model “hole” (Reason, 1990) was growing during these warmer months. To explain this, we assumed “experiential bias” (Johnston, 2013) from shifting factors (e.g., seasons) as a key culprit, requiring tasks at risk of failure to use a dynamic model. It appeared reasonable that the warmer it becomes, the less the care team thinks of infection checklists, and a chronic obstructive pulmonary disease (COPD) checklist is considered more (e.g., due to seasonal allergies).
Given this dynamic nature, CHRO offers a faster, more efficient way to load-balance the cognitive bandwidth of the available team to make its members more effective. This, in turn, prevents cases of sepsis and severe sepsis (e.g., at least 10 cases prevented in the pneumonia cohort itself, as month four saw only 16 total sepsis-related pneumonia cases, the lowest level all year), improves patient safety, and reduces the need for restricted antibiotics—in this case, 38% less than the number of cases expected. The overall result is seen in Figure 3. Finally, since pneumonia patients were administered 10.25% of all antibiotics in the hospital, the hospital’s estimated reduction of restricted antibiotics was determined to be 3.9% overall. 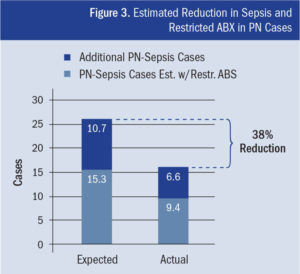
Finally, given the MHS-VA are health systems committed to HRO, we explored how CHRO aided troops and veterans. Wright-Patt’s (MHS) CHRO reduced failure to rescue (FTR) by 87%, and compliance, patient satisfaction, and efficiency (e.g., lowering readmissions) all improved (Wright-Patterson Medical Center, 2015). Troops’ and veterans’ lives were included—a 30% increase in census was attributable to Wright-Patt’s VA partners. Keesler AFB’s CHRO has already helped prevent FTR of five patients in one month. Furthermore, the civilian study hospital also had prevention of veteran FTR—one sampled month had 35 veterans as patients, with one receiving an alert. Ultimately, the same model applied for sepsis can also be applied to other critical MHS-VA issues, such as suicide (itself an FTR), since it optimizes the timing (Brennan, Malaspina, & Veluswamy, 2012) of task covering to balance urgency/effectiveness (i.e., not too late) and resource efficiency (i.e., not too soon) to feasibly achieve high reliability.
Conclusion
A “preventable” problem implies that correctly completing tasks on time may avoid the problem altogether. Most care tasks involve human thought, which is impaired by task saturation. Saturation can be prevented using a CHRO to predict potential failures and thus know where compliance will be reliable. This study concentrated on reducing the incidence rate of preventable sepsis (and its complications), and restricted antibiotic overuse for an antibiotic stewardship program. This method could also be readily extended into congestive heart failure, COPD, and any other diagnoses that have preventable complications.
Reliability enables facilities to achieve the high—yet safe—patient volumes required to improve patient access nationwide. However, this requires large gains in quality assurance productivity (i.e., force multiplication). To achieve these gains, a CHRO micro-targets quality assurance efforts away from areas of predicted reliability, thus preventing checklist overload of care teams, and ultimately improving value-based care without increasing staff.
The authors wish to thank the following:
Johns Hopkins Medical Center: Shereef Elnahal, MD, MBA, co-designer of the CHRO concept based on research at Wright-Patterson AFB, and Joseph Herman, MD, and Peter Pronovost, MD, PhD, for their pro bono contributions of their expertise to this project.
U.S. Air Force Medical Service: Major General Dorothy Hogg, for her support of the MAM during the CNS pilot program, and Lieutenant General Mark Ediger, for his support of the med-surg nurse consultant role.
Wright-Patterson’s 88th Medical Group: Col. Timothy Ballard, Col. Gregory Sweitzer, Maj. Aven Ford, Maj. Caelan Ford, John Bieghle, and Col. Penelope Gorsuch, as well as the 88th Medical Group team, for contributions to the first CHRO project’s success.
Saint Joseph Mercy Oakland/Trinity Health System: Jack Weiner, Morris Pajewski, Ramesh Madhavan, MD, and Connie Parliament, for contributions to the SJMO CHRO project’s success.
The High Reliability Organization Council: Eva Johannson, Aashka Shah, Ragupathy Veluswamy, and Terry Rajasenan, for the Council’s pro bono contributions to this project and article, for its expertise on MAM, and for its mission in making HRO become more ubiquitous.
The Pittsburgh VA Medical Center: David S. Macpherson, MD, MPH, Ali F. Sonel, MD, Suresh R. Mulukutla, MD, and Adrian A. D’Amico, MD, for sharing expertise in checklist overload and clinical approaches for addressing complex VA patients at Wright-Patt.
Lt. Col. Jared A. Mort, MSN, MBA, is a clinical nurse specialist and is responsible for the nursing care of all inpatient medical-surgical cases at Keesler (Mississippi) Air Force Base. He has over 19 years’ experience as a nurse, and during 2013, when deployed to Afghanistan as chief nurse of a Forward Surgical Team, he helped achieve a 99.5% survival rate. He also serves as medical-surgical consultant to the Air Force Surgeon General, consulting for 3,000+ nurses. He led the design of the CHRO while at Wright-Patterson Air Force Base in Dayton, Ohio.
Becky Alsup, BSN, RN, is the sepsis coordinator of St. Joseph Mercy Oakland (SJMO) in Michigan and a patient safety expert. She has 11 years of experience in nursing, with a background in critical care medicine. She is leading the CHRO/MAM project for SJMO and for Trinity Health System in infection time-to-treatment, as she has deployed MAM in the reduction of unexpected mortality successfully at SJMO.
Fabian Fregoli, MD, is vice president of quality and patient safety and chief medical informatics officer at SJMO and regional chief medical informatics officer-East market for the Saint Joseph Mercy Health System (part of the Trinity Health System). In addition to his focus on clinical quality and patient safety, Dr. Fregoli provides leadership in clinical informatics to the hospitals he serves. He is a clinical assistant professor at Wayne State University School of Medicine and the Michigan State University School of Medicine in the Department of Family Medicine.
REFERENCES
Barber, B. (2016, April 14). Wright-Patterson doctors, nurses improve care at hospital. My Dayton Daily News. Retrieved from www.mydaytondailynews.com
Brennan, J., Malaspina, M., & Veluswamy, R. (2012). A physician partnership: Employing predictive modeling and workload analysis for CHF performance improvement. American College of Physician Executives Update, September 20, 2012 (online).
Elnahal, S., Herman, J., & Pronovost, P. (2015). A tale of two systems: Combining forces to improve veteran and military health care. American Journal of Medical Quality, 31(3), 279–280. doi:10.1177/1062860615613581.
Elnahal, S., Moningi, S., Wild, A., Dholakia, A., Hodgin, M., Fan, K. … Herman, J. (2015). Improving safe patient throughput in a multidisciplinary oncology clinic: Managing task saturation to improve efficiency and quality. The Physician Leadership Journal.
Hall, M. J., Levant, S., & DeFrances, C. J. (2013). Trends in inpatient hospital deaths: National Hospital Discharge Survey, 2000–2010. NCHS Data Brief No. 118, March 2013. Retrieved from https://www.cdc.gov/nchs/products/databriefs/db118.htm
Johansson, E., Wilson, D., Mapson, C., Young, K., Littwin, S., Shallcross, L., Acquah, S. (2016). Enhancing human performance for better healthcare outcomes: Doing more with less. The Physician Leadership Journal, January 2016.
Johnston, R. (2013). Analytic culture in the U.S. intelligence community: An ethnographic study. Central Intelligence Agency. Retrieved from www.cia.gov
Pronovost, P., & Marsteller, J. (2014). Creating a fractal-based quality management infrastructure. Journal of Health Organization and Management, 28(4), 576–586.
Reason, J. (1990, April 12). The contribution of latent human failures to the breakdown of complex systems. Philosophical Transactions of the Royal Society of London B, 327(1241), 475–484. doi:10.1098/rstb.1990.0090.
Sun, L. H. (2016, June 6). Behind the scenes of a U.S. superbug discovery that made headlines around the world. The Washington Post. Retrieved from www.washingtonpost.com
Veluswamy, R. (2008). Golden nuggets: Clinical quality data mining in acute care. Physician Executive Journal, 34(3), 48–53.
Wright-Patterson Medical Center. (2015, December 1). Wright-Patterson Medical Center advancements in value-based care help lead the region. Wright-Patterson Air Force Base. Retrieved from www.wpafb.af.mil
