Health IT & Quality: Super-organism Focused Care
September / October 2012
![]()
Health IT & Quality
Super-organism Focused Care
About 10 trillion cells make up the human body. The joining of eggs and sperm at the time of fertilization brings together 23,000 genes. In a healthy gut alone, more than 100 trillion bacteria thrive.
Scientists estimate that the microbiome—the term used to describe all the bacteria and other organisms that live on and within us—collectively represent more than three million genes. These bacteria live symbiotically with us, providing a variety of beneficial protections while we offer them raw materials and a nice, warm shelter in which to grow and reproduce. For most of medical history, physicians studied disease states without consideration of the microbiome. Only recently have researchers viewed the human body as a super-organism, influenced as much by the genetics of the host as by the permanent bacterial residents.
Initial work on the microbiome shows that humans in different parts of the world harbor different microbiomes. Although we do not know why, the guts of children in rural Venezuela contain more riboflavin-producing bacteria than those from North America. These bacteria are very good at breaking down glycans as they produce large amounts of the enzyme glycoside hydrolase. Therefore, these children are better at obtaining nutrition from their mother’s milk than American children. Amazingly, children produce no glycoside hydrolase on their own, yet all mother’s milk contains glycans. Humans have evolved to take advantage of their microbiome while the bacteria similarly have done the same.
They Choose Us; We Them
The microbiome offers humans an expanded ability to thrive within their environment by offering additional functionality—such as breaking down complex carbohydrates—that would be difficult to code within our limited number of genes. Through evolution, bacteria chose us, and we chose bacteria, establishing a powerful, mutually beneficial relationship.
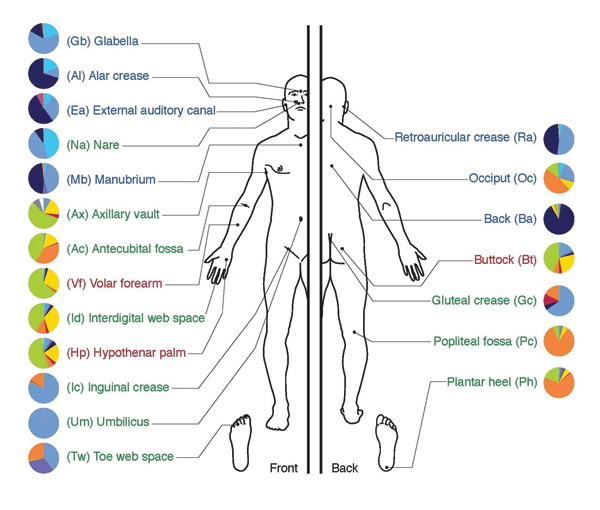
Bacteria, archaea, and fungi form the microbiome with bacteria being the most diverse and abundant. These organisms reside within the gut, conjunctiva, and skin (Figure 1). The metabolic activity of the gut flora approaches that of a typical human organ.
Bacteria constitute more than 60% of the dry mass of feces, making this waste product an ideal source to test gut flora for any descriptive characteristics or abnormalities. Recent advances in genetics now allow researchers to gene sequence the microbiome of the gut to understand its relationship to both health and disease.
Dr. Jeffrey Gordon of the Washington University School of Medicine in St. Louis, Missouri, completed some preliminary research suggesting that gut flora may have a significant influence on the risk for both obesity and malnutrition. Surely caloric intake is a very important factor in both of these diseases, but evidence is growing that the microbiome modifies the risk by shifting how calories are both processed and adsorbed.
Microbiome Causing Type 2 Diabetes
Work done at the Imperial College, London, and the Cleveland Clinic in Ohio provides evidence that the risk for Type-2 diabetes may be linked to the microbiome. As Type-2 diabetes is caused by the body’s insensitivity to insulin, is it possible an abnormal microbiome is producing chemicals that modify a human cell’s response to insulin? If the chemicals produced by the microbiome can help us absorb and utilize nutrients, it is not unreasonable to postulate that a mircrobiome gone haywire may harm us by changing the way we metabolize glucose.
Clostridium difficile, a bacteria commonly found in the human gut, is kept under control through competition with other harmless bacteria populating the colon. Only when that competition disappears does C. difficile morph into a lethal organism that kills more than 14,000 people in the Unites States each year.
When hospital patients suffering from infections receive antibiotics, the medication not only kills the offending organism, but also the healthy bacteria in the gut. If too much of the gut flora is eliminated, C. difficile, often resistant to many antibiotics, takes the place of all the healthy bacteria, leading to severe, life-threatening diarrhea. Logically, if the normal gut flora is protected from the antibiotics or replaced after treatment, the C. difficile would not have the opportunity to proliferate wildly throughout the colon and cause disease.
Researchers at Baptist Medical Center in Oklahoma City are experimenting with such an approach. C. difficile-infected patients receive enemas with feces from normal, healthy patients in an effort to repopulate the colon of ill patients with good bacteria. In 77 patients treated this way, the researchers achieved an initial success rate of 91% and a 99% success rate after two treatments.
Personalized Medicine
The field of personalized medicine promotes the customization of treatment for patients to the individual characteristics of each person. Recent work in genomics and pharmacogentics, driven by the sequencing of the human gene and subsequent technological breakthroughs that reduced the cost of such testing, provides ever increasing new medical knowledge that facilitates the delivery of personalized medicine. Expanding our focus to include the microbiome presents an exponentially larger challenge to understand the causes and treatments of disease. Invariably, researchers will unlock the secrets of the microbiome and the human super-organism. These secrets require our application of this knowledge to patient care to ensure the best possible outcomes.
Even today, the new medical knowledge produced in even narrow disciplines exceeds the capacity of any physician to assimilate and apply effectively. Adding the complexity of the microbiome only makes the task of assimilating the relevant medical knowledge further out of reach.
Health information technology offers clinicians tools to manage this avalanche of information. As new knowledge is obtained, this information can be codified in guidelines, order sets, and searchable knowledge bases, relieving physicians of the impossible burden of assimilating all this new information. Using intelligent clinical decision support delivered through equally intelligent and flexible clinical workflow, physicians will choreograph the use of this information to deliver personalized treatment to each of the their patients.
The deepening complexity of medical care, driven by the ever-increasing knowledge of biology, genetics, and disease, requires physicians to embrace the capabilities of information technology. It is the only way clinicians will be able to treat the super-organism known as man.
Barry Chaiken is the chief medical officer of DocsNetwork, Ltd. and a member of the Editorial Advisory Board for Patient Safety & Quality Healthcare. With more than 20 years of experience in medical research, epidemiology, clinical information technology, and patient safety, Chaiken is board certified in general preventive medicine and public health and is a Fellow, and former Board member and Chair of HIMSS. As founder of DocsNetwork, Ltd., he has worked on quality improvement studies, health IT clinical transformation projects, and clinical investigations for the National Institutes of Health, U.K. National Health Service, and Boston University Medical School. He may be contacted at bchaiken@docsnetwork.com.
