Patient Mobilization
March/April 2011
Patient Mobilization
Best practices improve health outcomes and ensure safety for patients and staff alike.
 |
|
| There must be adequate and appropriate equipment readily available for caregivers to be able to address specific patient movement. |
As research supports the critical need for mobilizing hospitalized patients, the adage “If you don’t use it, you will lose it” sums up the weakness and loss of functional status seen with prolonged bed rest. In the hospital setting, patients often depend on their caregivers for mobilization. The physical demands of mobilization on caregivers often places risk on both the patient and the caregiver. This article will explore how an effective safe handling practice will improve patients’ health outcomes, increase healthcare organizations’ profitability, and ensure caregivers’ safety.
In-Patient Early Mobilization Programs
Human mobility serves a greater physiological purpose than just transferring one’s self from one point to the next. Mobility helps us perform activities of daily living, express emotions, and gratify basic needs, as well as sustain our health and enhance our body’s ability to heal and repair. With bed rest or a dramatic reduction of mobility, the body systems most affected are metabolic (fluid and electrolyte imbalance), respiratory (hypostatic pneumonia), cardiovascular (orthostatic hypotension, thrombus), musculoskeletal (atrophy and contractures), urinary elimination (infection and dehydration), integumentary (pressure ulcers) and psychosocial (depression).
Positive Patient Outcomes and Cost-Saving Opportunities
Life experiences such as injuries, accidents, disease, and aging can change our ability to mobilize independently. Research illustrates the vital role mobilization has on the body’s ability to maintain functional independence as well as to sustain and heal from a negative health event. Because of this research, healthcare organizations are reducing the amount of time a patient spends on bed rest by integrating mobilization protocols into the plan of care.
Pressure ulcers are an example of how early mobilization programs can sustain a person’s health and save the hospital great expense. Typically, pressure ulcers result from prolonged periods of uninterrupted pressure on the skin, soft tissue, muscle, and bone. Pressure ulcers cause extreme discomfort to a patient and often lead to serious, life-threatening infections. In 2007, the Center for Medicare Services (CMS) reported 257,412 cases of preventable pressure ulcers as a secondary diagnosis. The average cost per case in which pressure ulcers were listed as a secondary diagnosis was more than $40,000 per hospital stay (AHRQ & Healthcare Cost and Utilization Project, 2008). In October 2008, CMS deemed pressure ulcers acquired during a hospital stay as never events, and therefore, provides no reimbursement for the cost of care. Research is showing that with an effective patient mobility program, a great many pressure ulcers can be avoided.
The biological reasons behind the positive effects of mobilization and the ability to enhance other patients’ health outcomes are not known. Physiologically, it is known that changing a patient’s body position from a horizontal to an upright position does increase heart rate, which has a positive impact on blood flow redistribution and aides in the delivery of drugs to the entire body. In the upright position, maximum lung expansion improves the ability to take deeper respirations, which increases oxygen intake. Whatever the reasons, research is validating that early mobilization substantially enhances a patient’s ability to heal.
As reported in “Early Mobilization of Patients in ICU Improves Outcomes,” (American Thoracic Society, 2009) 100 ICU patients in a randomized trial receiving mechanical ventilation with sedation were treated with an early mobilization protocol. The findings of this research validated that the mobilization of the ICU patients greatly improved their long-term recovery rates.
In another study, “Early Mobilization of Patients Hospitalized with Community-Acquired Pneumoniants,” (Mundy et al., 2003) 458 patients admitted for community-acquired pneumonia (CAP) during a 6-month period improved faster with early mobilization, as evidenced by reducing the length of hospital stay by 1.1 days. This study validates the positive impact that mobilization has on a patient’s health. Cost effectiveness provides tremendous motivation for healthcare organizations to integrate early mobilization programs into their standards of care.
Cost and Risk Exposure
As discussed above, early mobilization programs provide tremendous benefits for patients, however mobilizing partial and totally dependent patients imposes even greater risk of injury to caregivers, the most valued resource a hospital has. Current national statistics rank healthcare workers as the occupation experiencing the third highest number of work-related injuries. On average, a 250-bed hospital spends approximately $337,000 annually on caregiver injuries related to lifting, transferring and repositioning patients. According to the National Institute of Occupational Safety and Health (NIOSH), caregivers are at risk of injury if manual lifting demands exceed 35 pounds (Waters, 2007). The average American male weighs 190 pounds, and the average female weighs 160 pounds (Ogden et al., 2004). To expect caregivers to manually mobilize dependent or partially dependent patients even more frequently only intensifies this existing hazard.
Another cost and risk exposure for early mobilization programs is related to hazardous working conditions for caregivers: transfer-related patient falls. Based on the NIOSH study cited above, caregivers are not safe lifting over 35 pounds. If caregivers are not safe doing manual transfers, neither are the patients. CMS included patient falls as never events in October 2008 as well, so healthcare related to the treatment of injuries from a fall exposes organizations to significant monetary losses and, more importantly, negatively impacts patients’ health. In addition to a healthcare organization’s expense for the treatment of falls, patient falls are one of the leading triggers of professional liability claims, which can cost a healthcare organization between $25,000 and $19 million.
Best Practices
Currently, research is validating the patient benefits of early mobilization programs. Workers’ compensation statistics and the cost of patient transfer-related falls reflect the unrealistic demands of manual patient movement. Healthcare organizations that integrate safe handling practices into the care delivery process can integrate a best-practice approach to an early mobilization program.
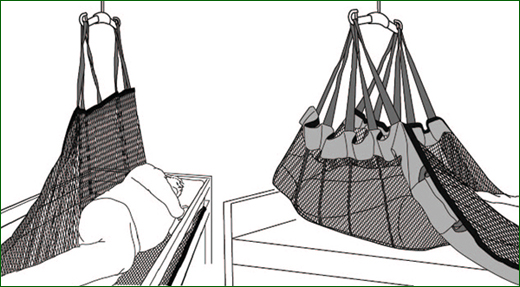
To ensure safe handling practices are a permanent aspect of the care provision, several key components must be in place. A safe handling policy and procedure must be in place to provide the overall structure of the practice. Care practices such as assessments, evaluations, and care interventions such as skin integrity, fall risk, and pain management must all integrate with the appropriate equipment to replace manual handling, which further communicates to caregivers the therapeutic need and benefits for patients. Support processes must be developed. These processes will help to sustain the integrity of the safe handling practice as well as identify opportunities for strengthening and evolving the practice as needed.
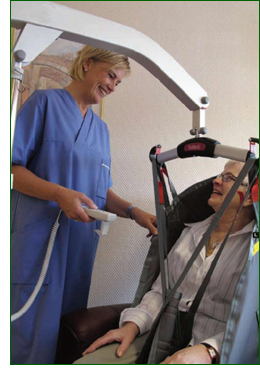
There must be adequate and appropriate equipment readily available for caregivers to be able to address specific patient movements. Training on the function and use of the devices is a critical part of building caregivers’ skills, but equipment training alone is not sufficient for caregiver competence and confidence. In addition to equipment training, developing caregiver compliance with the use of equipment is best accomplished when expert-level safe handling nurses can mentor these skills at the bedside. Working side by side with the caregivers to lift and transfer patients, the expert nurses teach by doing. Caregivers’ competence and confidence increase when the use of equipment on patients with clinical challenges such as ventilators, contractures, post-procedure limitations, and pain management issues is managed easily and efficiently.
A successful safe handling practice will enable caregivers to provide early, frequent, and safe mobilization for patients who are partially or totally dependant. The ability to provide this intervention without the risk of injury greatly improves patients’ ability to heal and dramatically reduces healthcare organizations’ financial exposure.
Summary
There is significant clinical impact on quality and cost of care, patient safety, and patient comfort when patient handling and movement are not properly performed. Early mobilization protocols can greatly benefit patients’ ability to heal and return to health.
A successful safe handling program can reduce the number and cost of caregiver injuries by at least 80%. The 250-bed hospital described above, where caregiver injuries related to lifting and transferring cost more than $337,000 per year, could save more than $270,000 annually with a safe handling program, as well as ensure its caregivers’ safety.
A safe handling program protects both the patient and caregiver during mobilization. To create the healthiest and safest healthcare environment possible, an effective early mobilization program is truly dependant on a successful safe handling program.
Barbara Peterson is the business development director for Risk Management Solutions (RMS), a healthcare consulting firm headquartered in Columbus, Ohio, that consists of a group of clinical professionals with expertise in all facets of the risk management field, including long-term care, acute care, rehab, home health, behavioral health, and other healthcare environments. For more information about RMS, visit www.rmsol.com. Peterson may be contacted at Barbara.peterson@rmsol.com.
Betty Bogue is president of Prevent, Inc., a registered nurse-led safe handling development service dedicated to providing healthcare organizations the resources, support, training, and mentoring to integrate the use of handling devices to safely lift, transfer, and reposition their clients. For more information about Prevent Inc. visit www.getalift.com.
References
