Partnership Improves OB Safety in New York State
July / August 2012
![]()
Partnership Improves OB Safety in New York State
Unique state initiative focuses on team training to standardize and manage EFM.
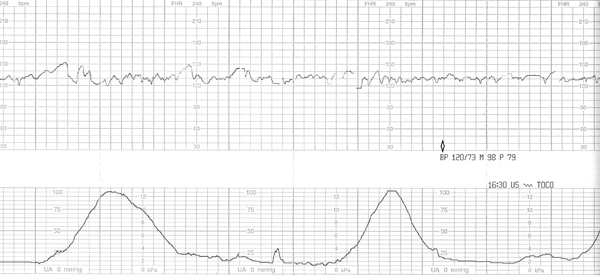
The safety of mothers and babies is paramount—and there have been significant technological advancements that help to ensure healthier babies and improved fetal outcomes. Although there are many avenues and approaches to obstetrical (OB) safety, in New York State a unique partnership between physicians and other clinicians, hospitals, and the state health department is focused on standardizing the definitions and interpretation of electronic fetal monitoring (EFM). A primary reason for targeting EFM is the fact that it is the most common method of intrapartum surveillance, used in approximately 85% of births. For more than 40 years, EFM has been employed to warn obstetric teams of potential fetal complications that may lead to injury, including brain damage or death.
Given the importance of EFM, the Healthcare Association of New York State (HANYS) partnered with the American Congress of Obstetricians and Gynecologists (ACOG), District II , and the New York State Department of Health (DOH) to develop and provide vital training on how to interpret, communicate, and effectively respond to fetal heart rate (FHR) tracings. Funded by a grant from the New York State Health Foundation, the primary goals of the initiative were to improve fetal outcomes in New York State by standardizing how obstetric team members interpret EFM results and discuss them with other members of their obstetric teams. Despite a decade of education and information on the standardized language for defining and classifying EFM parameters, variability has remained a challenge.
“We believed that standardizing the definition, interpretation, and management of fetal heart rate tracings among the entire multidisciplinary obstetric team would not only help to improve fetal outcomes in the state, but serve as a building block for other obstetric safety interventions in hospitals,” said Daniel Sisto, president of HANYS.
This is one of the first—perhaps the only—statewide partnerships among organizations that represent physicians, hospitals, caregivers, and the state regulatory agency to create and execute a statewide curriculum geared for multi-disciplinary obstetrical teams. This innovative statewide partnership served as the model for “on the ground” teams and training across New York State.
Focusing on multi-disciplinary collaboration in women’s healthcare is the beginning of what the future of medicine will hold,” said Donna Montalto, MPP, executive director, ACOG District II.
Employing Teams in a Straightforward Approach
Guided by a statewide EFM Task Force and funded by the New York State Health Foundation, New York State’s Obstetric Safety Initiative: Providing Excellence in Electronic Fetal Monitoring (OB Safety Initiative) recruited 86 hospitals and nearly 400 multidisciplinary OB providers from December 2008 through March 2011. Because physician engagement and leadership support were essential—as is the case in all safety initiatives—this initiative was led and co-chaired by a healthcare executive and physician leader. Joel Seligman, CEO, Northern Westchester Hospital Center, and Richard Berkowitz, MD, FACOG, co-chair of the EFM Task Force and professor of obstetrics and gynecology, New York-Presbyterian Hospital-Columbia University Medical Center, Division of Maternal Fetal Medicine, led the statewide EFM Task Force, which helped to design the initiative.
“It is crucial to have executive buy-in to quality and patient safety initiatives,” said Mr. Seligman. “As a CEO serving as co-chair of the EFM Task Force, we were demonstrating support from the top.”
“Our objective was to spread the word throughout the state to every individual—from physicians, midwives, and nurses to other members of the OB team,” said Dr. Berkowitz. “We enjoyed great participation of healthcare providers, large and small, from every corner of the state.”
Inclusion and teamwork were the foundation for this initiative and at the core of the curriculum developed by two nationally-renowned experts—David Miller, MD, FACOG, professor of clinical obstetrics, gynecology, and pediatrics, Keck School of Medicine, University of Southern California and Children’s Hospital Los Angeles; and Lisa Miller, CNM, JD, president of Perinatal Risk Management and Education Services.
The curriculum was based upon a standardized interpretation and management model developed by Ms. Miller and Dr. Miller, which incorporates the nomenclature of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). According to Ms. Miller, this model and the curriculum built for the New York state initiative recognized and addressed all the issues related to safety: lack of knowledge, lack of consensus, importance of teamwork and communication, and learning together. It accomplished this through a program of train-the-trainer education and learning, data collection and use, and communications and teamwork.
The Miller model looks at three basic elements related to EFM:
- Definition: What do I call it?
- Interpretation: What does it mean?
- Management: What do I do about it?
“Straightforward, simple, and practical” is Dr. Miller’s mantra when it comes to understanding and interpreting EFM. “EFM is used by everyone—newly graduated nurses, residents, seasoned doctors, midwives—so the information needs to be understood by people with diverse backgrounds and training. Because this involves so many caregivers, hierarchy needs to be flattened and there is a need for common understanding.”
An innovative feature of the OB Safety Initiative is its reliance on the training of multi-disciplinary teams in a train-the-trainer approach, which enables additional training and sustainability at each hospital. Unlike traditional education in healthcare—where doctors learn with doctors, and nurses learn with nurses—this initiative engaged teams from hospitals so that all those involved in EFM were learning the same nomenclature and techniques in the same room, at the same time. This makes a tremendous difference in both communication and teamwork within the OB unit at the local level.
“Engaging physicians and nurses and learning together is at the heart of this program,” said Lisa Miller. “Everyone who came to the program was engaged. For example, at the end of the sessions, box lunches were served and the participants were given the option to stay and brainstorm. An overwhelming number of physicians, nurses, and midwives stayed to brainstorm how to implement the training at their hospitals, in a collegial fashion. This is amazing since EFM interpretation has traditionally been the cause of some controversy and disagreement among healthcare professionals.”
“In virtually every bad outcome in every department, miscommunication and misunderstanding are at the root cause of a bad event,” said Mr. Seligman, co-chair, EFM Task Force. “That’s why we believe that collaborative learning is so critical.”
“Unlike other approaches to EFM training, we have tested the validity of our model through the collection of data,” said Dr. Miller. “We have information that demonstrates improved communications and perception of teamwork among hospital staff that participated in this program.”
“It’s got to be more than a one day program.”
One important point that was emphasized during the “train-the-trainer” programs is that teams must have plans to sustain learning and education including ongoing training, repetition, competency reviews, journal reviews, and ongoing review of fetal heart rate tracings. Success can only be accrued over time, it cannot be accomplished through a one-day program. Education has to be ongoing and repetitive.
The EFM initiative helped to sustain momentum for the participating hospitals after the initial training, which consisted of webinars, calls, and sharing of best practices. In addition, an EFM online toolkit was created to provide obstetric providers ongoing education and resources in EFM. This toolkit, available on the ACOG District II Web site, offers resources for education and training, self-assessment tools, reference and resource materials, books, articles, and websites. It also offers a step-by-step tutorial to enhance provider competency in standardized nomenclature, interpretation, and management of FHR tracings. (The toolkit is available at http://www.acog.org/acog_districts/dist_notice.cfm?recno=1&bulletin=3757)
Moving from Education to Practice
It’s early, but the statewide EFM initiative is showing some initial results. Throughout the program, hospitals reported data related to their culture of safety, perinatal indicators, and hospital in-house education programs. These data enable the development of comparative reports that hospitals use to benchmark themselves against peers. Among the key accomplishments are:
- A multidisciplinary group of approximately 400 OB providers were engaged in the train-the-trainer programs.
- Nearly 94% of hospitals implemented one or more practice improvements as a result of the Initiative.
- At least 382 OB providers in NYS are now certified in EFM by the National Certification Corporation.
- At least 38% of participating hospitals link EFM competency to clinical privileging and re-credentialing requirements.
- The safety culture was enhanced at participating hospitals, which reported significant improvements in team communications and collaboration.
But, these are just early results—the real impact will be evident over the long term.
With this in mind, HANYS’ approach to EFM education and training offers continual reinforcement through activities like daily rounding, visual reminders, and EFM strip reviews at department meetings. It was clear that standardized practices need to become part of “what we do, part of the culture.
While the aggregate data reveal that the New York initiative is beginning to make a difference, perhaps most telling are the interesting and unique ideas that hospitals are developing around EFM training and education, which they are sharing through best practices.
At Mercy Medical Center in Rockville, Long Island, the EFM safety initiative was incorporated into the organization’s Total Performance Plus (TPP) program, which began in 2007. The hospital sent four professionals to the EFM train-the-trainer program, and they brought back materials, introduced staff to the information, and rewrote policies and definitions.
All professionals on the Mercy OB unit were involved—physicians, staff nurses, midwives, and physician assistants (PAs). To acquaint all staff with EFM terminology and interpretation, Mercy held a series of multidisciplinary programs, from one hour to one day of training.
At Mercy, the focus on standardizing and managing fetal heart rate tracings has led to strip readings now incorporated into the twice daily rounds held as part of TPP program. These rounds include labor and delivery staff, neonatal/maternal/fetal staff, physicians, nurses, anesthesiologists, housekeepers, PAs—anyone who is part of the labor and delivery team and interacts with mothers and babies. They convene at 9 a.m. and 9 p.m. for white board rounds to discuss patients by using SBAR communications techniques, look at some strips, use proper terminology, and review the plan of care.
This same method of rounding is used when something changes. The charge nurse calls the staff together, and they talk about what’s changed and the plan of action.
There have been some demonstrable changes at Mercy as a result of their efforts in OB. “Nurses have more of an ability to recognize and document when something changes and can better communicate with physicians,” said Barbra Kahn, RNC, nurse manager, labor & delivery, mother/baby, NICU, and Mercy Medical Center. “We’ve also seen better communication between the NICU and the delivery room, and better organization of delivery. But, most important, we are seeing fewer adverse outcomes, which we believe comes from better communication.”
At St. Mary’s Hospital in Amsterdam, the OB Safety Initiative has helped to strengthen the hospital’s perinatal safety initiative as part of Ascension Health. One of the five major improvement goals defined by Ascension is collaboration on fetal HR monitoring for nurses, physicians, and patients.
“We received excellent resources from HANYS, and books authored by the Millers were given to participants,” said Julia Shafer, Director, Women’s Health, St. Mary’s Hospital. “Providing resources like these to every individual shows commitment and investment in staff and sends a clear message about our mission and vision in safety.”
The St. Mary’s team is starting to see c-sections normalize, with rates down to less than 18% for a primary c-section. This is a direct result of recognizing which FHR tracings need to be monitored and those that need to be acted on. “We now have more reliable and consistent care,” said Shafer.
“The EFM initiative has been particularly helpful for the team in interpreting tracings that were ‘in the middle.'”
As often pointed out, it’s the simple things that make a difference. At St. Mary’s, one simple action was to post a standardized document of definitions and categories on the unit.
St. Mary’s and Mercy are just two examples of how hospitals are instituting sustainable change to improve standardization and management of EFM. Other quality improvement methods noted by hospitals participating in the initiative include periodic chart reviews, reviewing EFM strips at department meetings, incorporating EFM strips in rounds, incorporating EFM in QA and peer review programs, and redistributing an EFM post-test.
Setting the Stage for the Future
Standardizing the interpretation and management of EFM is just one element of an overall OB safety program. But the multi-disciplinary education employed in this initiative can help reduce the challenges associated with physician engagement and improve the adoption and implementation of certain practice changes.
“We found that the folks in the audience were hungry and thirsty for improvement,” said John Morley, MD, former medical director, Office of Health Systems Management of the NYS Department of Health. “We certainly saw desire within the audience. Every person in healthcare, not just those within the audience, wants to do a good job today and continue to improve for tomorrow.”
“We don’t hear nearly enough about what we are doing to keep mothers and babies safe. This has been an opportunity to both make a difference and draw attention to an important OB issue,” said Joel Seligman.
Kathleen Ciccone is executive director of HANYS Quality Institute and co-director of the New York State Partnership for Patients. As executive director, HANYS Quality Institute, Ciccone directs and coordinates all association activities for HANYS’ membership related to quality oversight, performance improvement, and research initiatives. As co-director, NYS Partnership for Patients, Ciccone co-directs education and consultation programs with hospitals throughout the state to achieve national Partnership for Patients Goals of reducing hospital-acquired complications by 40% and preventable readmissions by 20%. She received her master’s degree from the State University at Albany and is currently completing her DrPH.
Christa Christakis is senior director of quality and research initiatives at HANYS where she formulates the advocacy agenda and strategies for quality-related regulatory and legislative initiatives that impact HANYS’ member institutions. She also directed New York State’s Obstetric Safety Initiative: Providing Excellence in Electronic Fetal Monitoring, a collaboration among HANYS, the American Congress of Obstetricians and Gynecologists (ACOG), District II, and the New York State Department of Health. Christakis received her master’s of arts degree in public affairs and policy (MPP) from the University at Albany’s Nelson A. Rockefeller College of Public Affairs and Policy.
Andrea Mathis is a principal research analyst with The DataGen Group where she conducts and supports data analysis of research projects and grant-funded collaborative projects. She is also involved with research and development activities relating to product development. She has bachelor of science degrees in chemistry and molecular biology from Clarkson University. Mathis also received a master’s of public health degree in epidemiology from the State University of New York at Albany and is currently a PhD candidate in infectious disease epidemiology.
Patty Montone Charvat has more than 25 years of experience in healthcare communications—from strategy development to full plan execution including research, public affairs, marketing, media relations, community outreach, and education—and has worked with hospitals, healthcare associations, patient safety centers, and other health-related organizations across the country. She began her career in the corporate communications and marketing division of the Healthcare Association of NYS, with her most recent position being vice president. Charvat may be contacted at cpcharvat@aol.com.
