Consumers as Partners
July / August 2010
Consumers as Partners
Empowering Patients and Families to Call for Rapid Response
Engaging patients and families as integral members of the healthcare team is an essential step in delivering high-quality, safe patient care. One approach for empowering patients and families being implemented in hospitals nationwide is to invite them to activate rapid response teams (RRTs) if patients show signs of physical deterioration or something doesn’t appear “quite right” with the patient.
The growth in RRTs came as a result of the Institute for Healthcare Improvement (IHI) 100,000 and 5 Million Lives Campaigns, which include RRTs as one strategy for enhancing quality and safety. Generally, the RRT consists of intensive care unit (ICU) personnel who can be summoned to assess and treat any patient outside the ICU who shows signs of deterioration and who may be at risk for cardiac arrest or death. Team make-up varies by hospital, but often includes one or more ICU nurses, a respiratory therapist, and a physician who can be called upon when needed.
Initially, only healthcare professionals could activate RRTs. But, with the inspiration of Sorrel King, whose 18-month-old daughter Josie died as a result of a series of medical errors, patients and families are being empowered to activate teams. Experience has shown that families are often the first ones to recognize that there is an issue or a patient is in distress and requires assistance. In fact, tragic stories like that of the death of Josie King may have been prevented if families were, or felt, free to call on a healthcare team for fresh eyes to assess a change in condition or circumstance.
Hearing Sorrel King say, “If I would have been able to call a rapid response team, I believe Josie would be here today,” led a number of hospitals to consider and implement Condition Help (Condition H). Among the most notable is the University of Pittsburgh Medical Center (UPMC), one of the first hospitals in the nation to initiate Condition H. Since implementation, UPMC has been sharing its success and lessons learned with other facilities across the country. Now, Maryland hospitals are moving to adopt this important and innovative approach.
Bringing Condition H Statewide: The Maryland Experience
While hospitals across the country may individually be implementing Condition H, the Maryland Patient Safety Center (MPSC) is offering support and resources to help all Maryland hospitals embed these programs as part of their RRT efforts. For one year, seven Maryland hospitals participated in a Condition H pilot program with implementation support from the Delmarva Foundation for Medical Care and funding from CareFirst BlueCross BlueShield. Their experiences are being shared with other hospitals and the lessons they learned are being used to create a tool kit that hospitals can use to establish their own Condition H program. In fact, in September 2009, more than 75 healthcare providers representing 22 hospitals were brought together by MPSC to learn about Condition H and the findings of the pilot program.
Drawing from the experiences of UPMC, pilot hospitals, and national experts, MPSC is providing support, communications tools, and education for implementing Condition H in hospitals across the state. The Center is collecting data on codes outside ICU, the number of Condition H calls made, the total number of RRT calls, and mortality data to help guide initiatives. A comprehensive tool kit will be available on the MPSC website, www.marylandpatientsafety.org, this summer.
Franklin Square Hospital Center and Upper Chesapeake Health System were two of the early adopters of Condition H in Maryland and participated in the MPSC pilot program.
“We started RRT very early, just a few months after IHI released the six strategies for the 100,000 Lives Campaign,” said Patricia Norstrand, MS, RN, BC, senior director, department of quality, risk, and safety, Franklin Square Hospital Center. “I heard Sorrel King talk about how her daughter might be alive today if Condition H was in place, and I knew it was something we had to do. But, we wanted to make sure we had RRT effectively in place before engaging patients and families.”
Six months after implementing RRT, Franklin Square introduced Condition H.
Likewise, Upper Chesapeake Health System in Maryland, a two-hospital system, adopted RRTs early. According to Nancy Howard, RN, Project Coordinator of Performance Improvement for the System, Upper Chesapeake wanted to make sure that the RRT program was successfully implemented before launching Condition H.
Although both hospitals have programs in place, their approaches for patient/family activation of Condition H are different.
At Franklin Square, patients and families call on the floor nurse when they need help. This has enabled the “triaging” of calls by the floor nurse, making sure that the calls are focused on patient deterioration, the true intent of the program at the Franklin Square Hospital Center, according to Norstrand.
While some assert that this approach may discourage patient and family engagement, Norstrand said it has been working well. In fact, she noted, there were three or four calls pretty soon after the program was initiated. A simulation of Condition H by Franklin Square on a local news station helped to inform public awareness and also resulted in two Condition H calls.
“Our philosophy is that patients should call whenever they need help,” said Howard of Upper Chesapeake. “Whether it’s a deterioration in condition, a communication issue, or simply confusion, patients and families can call the Condition H number and get help immediately.”
When a Condition H call is activated at Upper Chesapeake, the RRT team, composed of an ICU nurse and a respiratory therapist, go to the patient and assess the situation. If it is a medical situation, they initiate next steps. If it is more of a customer service-oriented call, then Guest Services is summoned.
Regardless of the way in which Condition H is activated — through the floor nurse or through a phone number — both hospitals are experiencing much more patient and family involvement and empowerment.
A challenge faced by both hospitals — no doubt all hospitals — is ongoing patient and family education and awareness of Condition H.
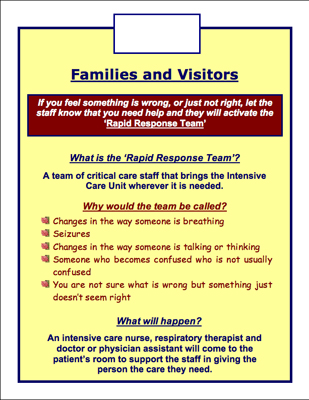
From the time of admission, patients and families are made aware of Condition H and how to activate the RRT if necessary. Through the use of posters and fliers in waiting rooms, nursing stations, and patient rooms, hospitals are maintaining visibility of the program. At Upper Chesapeake, these educational efforts are supplemented by having a sticker with the Condition H telephone number on the patient’s care plan folder, a flier within the folder, and a reminder about the program on the daily care plan sheet given to patients and families. In addition, signage that reinforces how to call the RRT is being hung in each patient room.
Franklin Square Hospital Center recently redesigned the posters for patient rooms (see below) and is now calling patients after discharge to assess awareness of Condition H and to determine if the posters are working. The good news is that a significant percentage of patients knew about the posters as well as the program.
Data are now being collected through the MPSC initiative on the number of Condition H calls vs. RRTs activated by hospital staff. Early results show progress is being made on patient/family initiation of calls. For example, at the 194-bed Upper Chesapeake Medical Center campus, there have been 323 RRT calls in 2009, ten of which were initiated by the patient or family member. At the 107-bed Harford Memorial Hospital campus, during 2009 there have been 150 RRT calls, three of which were initiated by the patient or family member. The Condition H calls related to pain management, perceived change in condition, and a perceived change in the delay of care.
Is Condition H making a difference in patient care and outcomes? Is it reducing mortality rates?
“Our goal has been to increase utilization of RRT, both patient/family and staff activated calls,” said Upper Chesapeake’s Howard. “We know that if we get to the patient early, when their condition is deteriorating, they may have a better outcome. Thus, an increase in RRTs and a decrease in codes outside the ICU will not only improve outcomes, but decrease total mortality rates.” To date, in addition to a reduced number of Codes occurring outside the ICU and a reduction in the inpatient mortality rate, Condition H calls have resulted in enhanced medication and pain management, transfers to higher levels of care because of changes in patient condition, and improved communication, according to Ms. Howard.
“Patient mortality has dropped considerably in the last two to three years, but we have so many patient safety initiatives underway that it’s difficult to pinpoint any one thing making it happen,” explained Norstrand. “However, I am certain that RRTs and Condition H are making an impact.”
There have also been unanticipated benefits of the Condition H program for the hospital, said Ms. Norstrand, including staff satisfaction.
“You can’t measure how important it is for a staff nurse to know that there is a team to help, especially for new staff and graduates,” she said. “There is a great sense of comfort that comes with Condition H and RRTs for staff as well as patients and families. In fact, rapid response has become a verb in our hospital, as in ‘we’re going to rapid response them.’” It also leads to important conversations between the care team and patients and families, offering the opportunity for early recognition of changing patient care needs.
RRT and Condition H have led to a new appreciation of roles and teams within the hospital, according to Norstrand. “By working together through RRT, the medical/surgical nurses and staff and the ICU nurses and staff have a greater appreciation of the skills and roles of each other as part of the patient care team,” she said.
Condition H is just one avenue for engaging patients and families in patient safety initiatives — but it is an important first step that is clearly making a difference.
Inga Adams-Pizarro joined the Maryland Patient Safety Center in 2008. In her role as director of operations and development for the Maryland Patient Safety Center she participates in strategic planning, fundraising, and organizational management efforts with the Center and its partners.
Tennille Daniels is a project manager with the Delmarva Foundation in Columbia, MD. Her responsibilities include serving as the project director for the Condition H Collaborative. Tennille received her masters in public health from Emory University in 2004 and has since dedicated her career to improving healthcare quality and patient safety.
Patty Montone Charvat has more than 25 years of experience in healthcare communications — from strategic communication planning to community outreach and education—and has worked with hospitals, healthcare, associations, patient safety centers, and other health-related organizations across the country.
