Integrating Biomedical Devices Across the Enterprise? Go with the Flow
November/December 2013
![]()
Integrating Biomedical Devices Across the Enterprise? Go with the Flow
When planning for biomedical device integration (BMDI), go with the flow—the workflow. Existing clinical workflow should be the guiding force to help improve patient safety, ensure efficient implementation, promote rapid and cost-effective adoption, and maximize hospital-wide benefits. As Sentara Healthcare discovered, involving clinicians themselves and all non-clinical departments that touch the technology can enhance workflow goals and streamline project management from multiple perspectives.
At Sentara, BMDI has been a successful multi-staged effort since 2006. It has reaped improvements in patient safety by providing more accurate data for analysis and alarm notifications and improved efficiency with documentation. The hospitals are also enjoying the benefits of real-time data delivery to the patient charts and meeting the requirements for Meaningful Use.
BMDI Defined
What is BMDI, and how can it help hospitals master today’s difficult challenges of creating more robust patient records and doing more with less? For the uninitiated, BMDI is an approach to directly deliver biomedical device data into the electronic medical record (EMR) system. Without it, data—especially vital signs—must be recorded on paper charts and duplicated through manual keying into the patient’s electronic record. BMDI eliminates these repetitive efforts and enhances the accuracy and efficiency of data communication. It improves clinical decision-making and enables clinicians to capitalize on more time with patients.
Through BMDI, biomedical devices are directly attached to the network and connect to a server equipped with an appropriate device driver. This server, functioning as middleware, transforms data as the EMR requires. Following this, an EMR enterprise integration engine delivers information seamlessly in the correct format to the patient record, with safety checks in place. In addition to patient monitors, our advanced BMDI system supports many types of medical devices, from ventilators to anesthesia machines and dialysis equipment, across most major vendors.
Given this, BMDI is leading Sentara into a scalable, safe, productive future for implementation of our high-priority EMR initiative.
Sentara Healthcare
Ranked as one of the nation’s top integrated healthcare systems, Sentara comprises more than 100 sites across Virginia and North Carolina, including 10 acute care hospitals, 8 that currently utilize BMDI. Five stand-alone emergency facilities also currently take advantage of the technology.
Our BMDI scope from 2006 to August 2011 primarily involved physiological patient bedside monitors, fetal monitors, and ventilators—the devices most often involved in integrations—in a wide range of settings for our nursing workflows. This included the ICU, labor and delivery, PACU, pre-op and post-op, ambulatory surgical center, endoscopy, and emergency departments. Since that time, we have also successfully completed integrating our anesthesia machines in surgical departments. Integrating entire hospitals, many with stand-alone emergency departments and ambulatory surgical centers, is no small task. Every department has its own set of device integration wants and needs.
Currently, our BMDI scope includes more than 2,000 biomedical devices of various types for 1,400 beds and has been met with great success. The nursing workflow alone generates more than 675,000 messages daily, after discarding the unnecessary data before sending it to our EMR.
In addition to using the native integration modules from our primary physiological monitor vendor when appropriate, we also selected Capsule Tech, Inc., as our BMDI integration provider because it offered the most flexible system available—definitely not a one-size-fits-all solution. The system architecture can be configured to meet specific department workflow and system needs and provides device drivers for hundreds of devices across most major vendors. This allows clinicians the flexibility to choose their preferred endpoint devices today and to add new ones in the future.
The Benefits of a Team Effort
From the integration launch, a dedicated full-time BMDI team has assumed overall responsibility for project management. These responsibilities range from developing a master project blueprint and reproducible models for specific departmental integrations to reviewing all device/network integration with our physiological monitor vendor as well as interfacing the BMDI solution with the EMR. Initially, the team consisted of three members. Since 2009, it has grown to five, which includes a manager, a system team coordinator, a senior system administrator and two system administrators. This is in part due to device growth but also additional responsibilities being added to the team.
Because of the numerous departments involved in the enterprise-wide project, we have been working directly with stakeholders to help gather the required data, coordinate efforts, and facilitate cross-department communications. As part of its responsibilities, the BMDI Team also helps bridge the gaps among these supporting teams.
This approach has served us well throughout all phases of the project, and any site planning biomedical integration deployment would be well served to follow a similar plan.
While not an all-inclusive list, Figure 1 shows how the BMDI Team bridges the gap between the various support teams throughout the device integration life cycle.
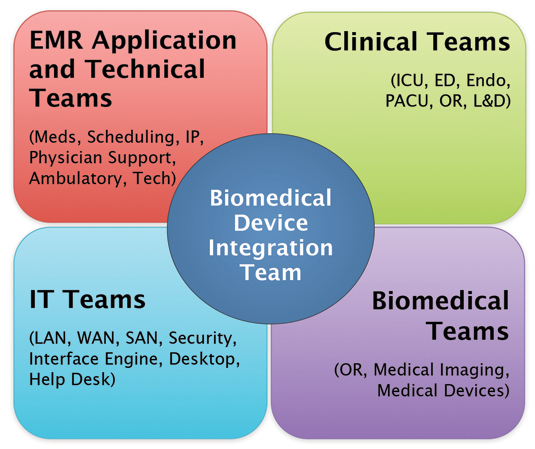
Figure 1. Biomedical Device Integration Team
The EMR Application and Technical Teams (top left) contain our meds, scheduling, IP, physician support, ambulatory, and EMR technical groups. The EMR teams provide the required device variables, confirm the clinician’s workflow and ensure correct patient record field mapping is completed from the enterprise interface engine so that information flows appropriately and displays correctly in the patient’s chart.
Our Clinical Team (top right), known as our super-users, includes clinicians from the various hospital departments whose devices are involved in the integration—the ICU, ED, endoscopy, OR, and labor and delivery. The BMDI Team works closely with this group to ensure that the system will efficiently support their workflows. Additionally, by understanding their workflow and device information, we can determine how to best implement the project to conserve expense and resources, while meeting their needs.
The IT Team (bottom left) includes the personnel responsible for LAN, WAN, security, EMR interface engine, desktop, and help desk. Because we are connecting equipment that has never before been installed on the network, keeping them informed of the process and understanding their requirements is important. The interface engine team, in particular, makes sure the enterprise EMR gateway connects appropriately with the EMR, while our LAN team manages the physical and virtual servers running our integration software.
Our Biomedical Team (bottom right) involves OR, medical imaging, and medical device teams, to name a few. Members of this team are the equipment experts and are able to provide an inventory of all current devices, including specific makes and models. They also manage any required device upgrades, hardware additions, and resolution of regulatory issues. We work directly with this team when configuring equipment to communicate on the network and to help us when troubleshooting support issues.
Each team requires motivated staff, ready, willing, and able to roll up their sleeves and communicate with others for go-live and subsequent challenges. Only with strong leadership and the buy-in of all team members are the optimal outcomes achievable.
Project Planning
As a first step in planning each phase of the project, our BMDI Team discusses specific needs with the EMR, Clinical, and Biomedical Teams and specific vendors if needed. This provides us with an overview for device specifications, frequency, and type of data to be documented as well as existing workflows. We provide the EMR team a list of variables that each device is capable of capturing for their refinement, based on what is required. If we determine that legacy devices and peripherals need to be replaced, we work with the biomedical and clinical teams in each clinical setting to determine the best course of action. Identifying these issues early on is important because of the length of time it could take to resolve the situation.
Our team takes onsite walkthroughs with the clinical and biomedical teams if needed to view the departments firsthand, discuss equipment location, and verify all information—which is key to an effective project plan. In this plan, it is imperative to allow ample time prior to the go-live for any possible complications—and, most important, for pre-implementation testing.
After we have previewed the devices in our test environment, we review with the EMR Team all the variables that can be captured and confirm that the unit of measurement used for each variable is appropriate for the EMR for each device type. It is important to note that not all machines can send every variable expected in the EMR and therefore some manual input may be required following the integration.
Understanding this is important to manage clinicians’ expectations or to work with departments on budgets for upgrading of these devices.
Once we have completed our testing and determined that all systems are functioning correctly, we schedule a go-live date and communicate with all the teams involved. For smaller scale integrations, we provide onsite support for a few hours. Larger scale integrations may need onsite support for up to a week.
Throughout the entire BMDI projects, we have been able to communicate effectively with each team and gather all the requirements for a successful integration. Bridging the communication gap between the groups is important because rarely do all the teams communicate directly with one another. From our observations, we have seen good communication between the Clinical and Biomed Teams, dealing jointly with point- of-care devices. Our Clinical and EMR Application Groups get together to discuss the application functionality and workflow issues. The IT and the EMR Application Committees collaborate on system and network requirements, and occasionally the Biomed and the IT groups discuss clinical devices on the network. However, there is little need for the EMR Team to work directly with the Biomedical Team or the Clinical Team to work directly with IT. Having the BMDI Team work with all teams to translate what is needed has improved efficiency and reduced frustration.
Additionally, we also have been drawing on the support of our existing Physician Advocacy Groups (PAGs), which helped guide implementation from the physician’s point of view and ensured that the specific information needed was integrated into the EMR. PAGs also played a role in fine-tuning equipment implementation and resolving conflicting requests at different sites throughout the enterprise. For example, prior to installing the anesthesia integration, we held a PAG Fair to obtain feedback on various monitor configurations to make the optimal choice for equipment setup.
Technology Specifics
For our physiological and fetal monitors, from the beginning, we have been heavily vested in the Philips Intellivue and GE Coreometric line respectively, but we also have a number of older Datex Ohmeda and GE Solar monitors. For ventilators, we have Hamilton Galileo and G5 Maquet Servo-i, Philips V60, and Puritan Bennett 840 ventilators. For the Epic anesthesia integration project, we added the anesthesia machines. This list includes Datex-Ohmeda Aestiva, Aespire, Draeger Apollo, and Narkomed machines. All are integrated with our EMR.
All of the devices that our BMDI team supports, other than Philips monitors, are managed through our Capsule endpoint agnostic middleware system and are integrated into the network through the Capsule terminal servers. In total, we employ over 400 four- and eight-port terminal servers. Capsule’s list of supported devices is robust, and we have only experienced one instance where a driver for a piece of our equipment was unavailable. The driver was developed, tested, verified, and validated, which allowed us to go live with the equipment shortly thereafter. In situations where central surveillance is not needed, we also have integrated several Philips monitors through their system.
We installed the Capsule software on virtualized servers in the Sentara data center. Currently eight of these virtual servers are dedicated to nursing and four to anesthesia. For the nursing servers, we decided to separate them by the eight facilities that were live on our EMR.
By contrast, for our Philips device integration, we use the HL7 functionality provided by the Philips servers to send the messages to our interface engine. To date we have configured this on 34 Philips’ database servers.
Data from both Capsule and Philips’ systems feeds into our Enterprise Interface Engine that transfers it to the EMR. This successfully accomplishes one of our major goals—data management through a single point-of-entry.
Supporting Departmental Workflows
Because the individual workflows and devices employed in each specialized department were similar enterprise-wide, our BMDI blueprint developed at the beginning of the project could be rolled out almost identically as the implementation expanded. The project, technology and workflow interaction is a two-way street. BMDI supports the way clinicians work, and at the same time the integration makes the most of the technology’s capabilities to minimize costs and maintaince.
Fixed Bedside Devices
In high acuity areas, such as the ICU, BMDI needs to support multiple devices in addition to the patient monitors. Here, Capsule four-port terminal servers are permanently attached to the headwall of each bed. When patients are admitted to a bed in the EMR, all the devices are attached. At that point, the vitals start flowing from the devices and into a flowsheet that contains invalidated vitals. The clinician can then go into that flowsheet and validate the desired vitals. It’s that simple.
If mobile devices are rolled into the room at a later point, clinicians simply plug these devices into a free port and a green light provides reassurance that all data is transferring as it should to the EMR.
Though we used four-port terminal servers in the ICUs, labor and delivery was a different case. Here, we found that only one device, the fetal monitor, was involved in bedside care. Therefore, we placed the four-port terminal servers in a central location and split the ports among two or three rooms to pare down hardware purchases.
Mobile / Non-Fixed Devices
Contrasting with this fixed device workflow, we also have mobile device workflow that typically involves anesthesia machines in the OR, various monitors in the PACU, and endoscopy departments, whether treatment is on an in- or out-patient basis. In Sentara’s anesthesia and surgery departments, the required biomedical devices are already physically mounted on the anesthesia machines and are plugged into a Capsule terminal server, which is also attached to the anesthesia device. Additionally, the anesthesia machines have a PC and touch screen monitor attached, which are used for EMR documentation. An association between the PC and the devices attached to Capsule terminal server mounted on the anesthesia machines is configured when setting the records up in the EMR. When an anesthesiologist starts an intra-op procedure in the EMR application running on the attached PC, all of the devices attached to the anesthesia machine are associated with the patient record with a single click. The device data then flows into the EMR as validated.
Another general integration scenario is employed for patients who are not admitted to a hospital bed. These may include certain endoscopy, PACU, and outpatient cases. For these cases, the clinician opens the patient’s chart and attaches the specific biomedical device to the patient, which will allow the data to flow until the device is removed from the patient or attached to a different patient in the EMR.
In our Sentara hospitals, some of the physiological monitors are wireless and have the capability to be employed in other departments with non-fixed workflows. Again, the clinician must individually associate each of these devices with the patient by opening the patient’s chart and selecting the correct device. While slightly more time-consuming, this significantly pares down the equipment and IT infrastructure involved and supports the workflow already familiar to the departments. An example of this is our endoscopy workflow. At the beginning of the procedure, the wireless device is attached and associated to the patient when they are in pre-op, the device travels with them to the procedure room and into post-op, with vitals continuously flowing into the EMR the entire time.
The Future
The BMDI team is always looking for opportunities to integrate devices in areas where frequent documentation of vitals is required. We expect device integration requests to continue to increase as more biomedical devices provide the capability to integrate with the EMR. We recently completed integration of our dialysis machines and in the future, we are looking at integrating ultrasound machines, smart pumps, and smart beds.
As the manager of connection and integration architect, Mike Freeman manages several IT teams at Sentara Healthcare, including the Biomedical Device Integration Team. During his tenure at Sentara he has overseen many projects that include the Biomedical Device Integration Team’s integration of more than 2,000 biomedical devices into their EMR at 8 of Sentara’s 10 acute hospitals. The implementation includes the ED, ICU, OR, L&D, PACU, and ENDO departments, with the number of devices and departments growing as integration opportunities arise. As an industry thought leader with more than 14 years of experience in information technology—12 years specifically in healthcare IT—Mike has presented on the topic of biomedical device integration at the national HIMSS event, AAMI, and a Healthcare Informatics webinar. With a BSBA degree in management from Christopher Newport University in Newport News, Virginia, Freeman has also achieved his MCSE (Microsoft Certified Systems Engineer), CEH (Certified Ethical Hacking) and Epic Workstations certifications.
Copyright © 2013 by Mike Freeman. Permission granted to Lionheart Publishing, Inc. to publish and use.
