Guided Reflection: A Strategy to Reduce Patient Falls and Fall-Related Injuries
By Cassandra Vonnes, MS, ARNP, GNP-BC, AOCNP, FAHA, Tina M. Mason, ARNP, MSN, AOCN®, AOCNS®, Jane Fusilero, RN, MSN, MBA, NEA-BC
According to the CDC (2013), one in three older adults fall each year. Although older adults are at an increased risk for falls and related injuries, those with a cancer diagnosis are even more at risk (Capone, Albert, Bena, & Tang, 2013; Stone, Lawlor, Savva, Bennett, & Kenny, 2012; Overcash & Beckstead, 2008). Studies have shown that falls occur in about 33% of older adults with cancer versus 29% of those without cancer (Spoelstra, Given, & Given, 2013).
Our center, the 206-bed Moffitt Cancer Center in Tampa, was still experiencing falls despite having a comprehensive fall prevention program in place. Prior to implementing the AHRQ (2013) fall prevention toolkit the same year of the toolkit’s release, we recorded 160 patient falls. After our nursing division implemented the toolkit, we recorded 143 patient falls. While this was an improvement, we conducted a literature review to determine if there were additional interventions that could have even more impact.
Hoke and Guarracino (2016) adopted a post-fall self-reflection on what could have been done to prevent a patient fall on an inpatient cardiac unit. This study included an after-event email crafted by the direct care nurse describing the fall. In addition to post-fall huddles, guidelines for assisting and remaining with high-risk fall patients during toileting and reinforcement of staff accountability aided in decreasing falls by 55% and falls with injuries by 72%. Mantzoukas (2008) defines reflection in the context of nursing practice as a process of transforming unconscious knowledge and practice into conscious, explicit, and logically articulated knowledge and practice. This allows for transparent and justifiable clinical decision-making. Reflection is the ability to create and clarify the meaning of an experience (Forneris & Peden-McAlpine, 2007).
Past process: When an inpatient fall occurs
As part of a comprehensive fall program using the national fall safety bundles, our center is required to have a post-fall huddle and post-fall assessment after each event. In our previous process, inpatient falls were reviewed at interprofessional bimonthly meetings. These meetings, which were established by the vice president of patient care services/chief nursing officer, included nurse managers, directors, physical therapists, a safe patient handling and mobility supervisor, clinical nurse specialists, and senior nursing leadership. During these “Fall Friday Reviews,” a safe, nonpunitive environment was created for discussing and learning about the events surrounding a fall. This was designed to be a fact-finding discussion, rather than a fault-finding one. Initially, nurses’ contributions were minimal—they were able to describe details around the event of the fall, but could not provide insight into contributing factors. The meetings also brought to light an inability to communicate concisely about the events, omission of key environmental or patient characteristics, and inconsistent reports among staff members. There was no formal opportunity for staff to evaluate their own practice related to the patient fall. The post-fall huddle interventions were single, drop-down box choices that did not allow any elaboration for practice change.
Guided reflection
After reviewing the literature, our team implemented a guided reflection policy to enhance the information shared at the Fall Friday Reviews. The geriatric nurse practitioner and Fall Friday Reviews chairperson created a data collection instrument to assemble variables associated with each fall, including the geriatric domains, in preparation for each meeting. These variables were identified in a systemic review of older adults with cancer (Wildes et al., 2015). Data that was collected originally around inpatient falls and associated with delirium began to be utilized in presenting fall data throughout the organization. This also led the cancer center to invest in remote visual monitoring, which became an intervention for injury reduction.
The utility of the reflective fall report was also expanded to prepare staff nurses, under the guidance of the geriatric nurse practitioner, to organize their account of a fall in preparation for the Fall Friday Reviews. Reports included background information, such as age, primary diagnosis, medications, and pertinent past medical history, to provide context to the oncology patient’s fall. This aided the nurse in identifying potential contributing factors that were not evident in the fall risk tool. Required documentation, such as fall risk score, injury risk, interventions, and patient family education, was included in the guided reflection to give the nurse an opportunity to review practice. Our fall risk score instrument has strong psychometric properties and was used historically to identify patients at risk, but not cancer patients specifically. Oncology patients have additional variables placing them at risk for falls, such as neurotoxic chemotherapies resulting in peripheral neuropathies. With this in mind, oncologic risk factors were added to assist the nurses and personalize the critical thinking piece of our risk assessment tool.
During the Fall Friday Reviews meetings, the direct care nurse reporting a fall or caring for the patient at the time of the fall presents the case, discussing contributing factors and potential gaps in care. Improved delegation and nurse accountability has decreased gaps in care and increased collaboration between the nurse and oncology technician. Meeting participants note they are more comfortable with their reporting (Table 1), and their presentation guides the listener through the post-fall review process by including pertinent background information. Feedback from nursing leadership and interprofessional team members has been overall positive. Since implementation of guided reflection, both falls and fall-related injuries have decreased (Figures 1 and 2).
Fall Friday Reviews in conjunction with guided reflection provide a collegial venue for evaluating patient falls with a focus on identifying causes, contributing factors, and preventive measures. Key findings and discussion points from the meetings are summarized for all staff in a biweekly Friday Fall Reviews bulletin.
Implications for practice
Falls and fall-related injuries in oncology patients are complex iatrogenic events. In the context of the fall event, reflection can be described in an iterative dimension as reflection is triggered by experience, which then produces a new understanding and the ability to act differently in the future (Mann, Gordon, & MacLeod, 2009).
Guided reflection allows the staff to assimilate more aspects of the event into a fuller picture for presentation. Common fall-related themes have been noted that would not have surfaced in traditional assessment and documentation. For example, the act of patients donning underwear—leaning forward and attempting to stand on one leg—has contributed to falls, as have patients getting up from chairs. The deeper dive into the nurses’ reflection of events and the sharing of stories revealed these themes. Subsequently, interprofessional collaboration, such as occupational therapy consults, may lead to decreased falls at home or fewer hospitalizations. Next steps include conducting qualitative research for inpatient RNs that have participated in Fall Friday Reviews with more direct thematic impressions of the guided reflective practice.
Table 1. Anecdotal Feedback of Participants
| “I feel as if I have all the pieces now to present a complete picture of the fall event. Guided reflection has improved my critical thinking and practice.” |
|
“It wasn’t bad at all. I felt prepared to present my patient and discuss with the group suggestions for next time.” |
|
“After completing the reflection worksheet, I was ready to tell the events of my patient’s fall. I even stayed to listen to the other presentations and I learned a lot.” |
|
“At first, I felt scared and a little intimidated, but after I started presenting, I realized I knew all of the questions by filling out the reflection worksheet.” |
Figure 1. Inpatient Falls by Year
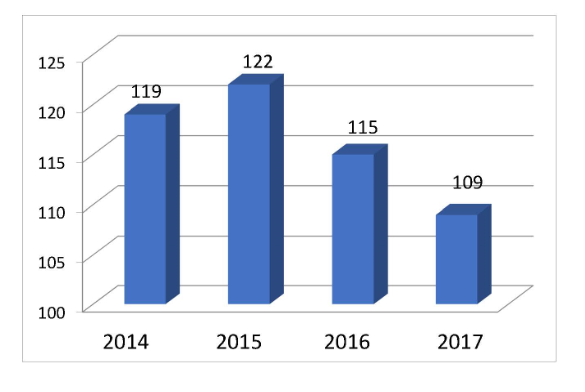
Guided reflection implemented in 2015 for Fall Friday Reviews.
Figure 2. Inpatient Level of Injury per Year
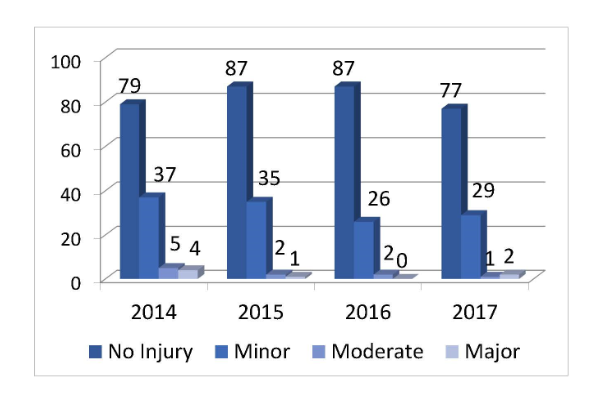
Guided reflection implemented in 2015 for Fall Friday Reviews.
Cassandra Vonnes is the NICHE coordinator/geriatric nurse practitioner in the Department of Nursing Professional Development, Tina Mason is the nurse researcher in the Department of Nursing Research, and Jane Fusilero is the vice president of patient care services and chief nursing officer. All three work at the Moffitt Cancer Center in Tampa.
References
Agency for Healthcare Research and Quality. (2013). Preventing falls in hospitals: A toolkit for improving quality of care (AHRQ Publication No. 13-0015-EF). Retrieved from https://www.ahrq.gov/sites/default/files/publications/files/fallpxtoolkit.pdf
Capone, L. J., Albert, N. M., Bena, J. F., & Tang, A. S. (2013). Serious fall injuries in hospitalized patients with and without cancer. Journal of Nursing Care Quality, 28(1), 52–59. doi:10.1097/NCQ.0b013e3182679056
Centers for Disease Control and Prevention. (2013). Costs of falls among older adults. Retrieved from http://www.cdc.gov/HomeandRecreationalSafety/Falls/fallcost.html
Forneris, S. G., & Peden-McAlpine, C. (2007). Evaluation of a reflective learning intervention to improve critical thinking in novice nurses. Journal of Advanced Nursing, 57(4), 410–421. doi:10.1111/j.1365-2648.2007.04120.x
Hoke, L. M., & Guarracino, D. (2016). Beyond socks, signs, and alarms: A reflective accountability model for fall prevention. American Journal of Nursing, 116(1), 42–47.
Mann, K., Gordon, J., & MacLeod, A. (2009). Reflection and reflective practice in health professions education: A systematic review. Advances in Health Sciences Education: Theory and Practice, 14(4), 595–621. doi:10.1007/s10459-007-9090-2
Mantzoukas, S. (2008). A review of evidence-based practice, nursing research and reflection: Levelling the hierarchy. Journal of Clinical Nursing, 17(2), 214–223. doi:10.1111/j.1365-2702.2006.01912.x
Overcash, J., & Beckstead, J. (2008). Predicting falls in older patients using components of a comprehensive geriatric assessment. Clinical Journal of Oncology Nursing, 12(6), 941–949. doi:10.1188/08.CJON.941-949
Spoelstra, S. L., Given, B. A., & Given, C. W. (2012). Fall prevention in hospitals: An integrative review. Clinical Nursing Research, 21(1), 92–112. doi:10.1177/1054773811418106
Stone, C. A., Lawlor, P. G., Savva, G. M., Bennett, K., & Kenny, R. A. (2012). Prospective study of falls and risk factors for falls in adults with advanced cancer. Journal of Clinical Oncology, 30(17), 2183–2133. doi:10.1200/JCO.2011.40.7791
Wildes, T. M., Dua, P., Fowler, S. A., Miller, J. P., Carpenter, C. R., Avidan, M. S., & Stark, S. (2015). Systematic review of falls in older adults with cancer. Journal of Geriatric Oncology, 6(1), 70–83. doi:10.1016/j.jgo.2014.10.003
