Communication Determines Patient Safety
By Cristina Vaz de Almeida
Communicating effectively allows us to clearly mark risks and measure patient safety limits.
Partnerships with the patient start with cooperation and commitment, where the health professional must be close to the patient to act as a true “observer.” Observation allows the clinician to assess the patient’s needs and “essence” (Egener & Cole-Kelly, 2004), enabling the relationship to grow and promoting favorable health outcomes.
Ricciardi & Shofer (2019) highlight the need for patients to be involved in their care by asking health professionals about their diagnosis and treatment through an open dialogue. When patients are involved as partners, they can detect adverse events and ensure safe care as well as promote a safety culture.
One of the public health doctors who participated in an in-depth interview for this paper says, “It is undoubtedly very important to develop communication skills in all their transversality, both verbal and nonverbal communication techniques, and I stress again the delivery of reminders/recipes/visual schemes that support the message conveyed.” To this doctor, verbal and nonverbal communication are critical to establishing effective trust and information exchange.
There are also useful tools that promote interpersonal relationships. The Agency for Healthcare Research and Quality (2019), for example, has “My Questions for This Visit,” a simple and effective card that gives patients a list of questions to ask during the medical meeting, such as:
1) What are my medications?
2) What tests and analyses do I need?
3) What surgery should I undergo?
The AHRQ Health Literacy Universal Precautions Toolkit, Second Edition, enables an intervention in primary care practices by seeking to reduce the complexity of healthcare; increase patient understanding of health information; and produce improvements in patient support at all levels of health literacy (Brega et al., 2015).
Several surveys show that up to 75% of hospital readmissions could be prevented by interventions aimed at greater patient and family involvement and cooperation, such as health education; pre-discharge assessment and coordinated home care; and family and patient-centered care (Mitchell, Heinrich, Moritz, & Hinshaw, 1997).
The subject of patient safety arose from the healthcare quality movement, which has been defined by the Institute of Medicine as “prevention of harm to patients” (Aspden, Corrigan, Wolcott, & Erickson, 2004). Emphasis is placed on a healthcare delivery system that avoids mistakes and learns from those that occur, based on a safety culture involving healthcare professionals, organizations, and patients.
The AHRQ Patient Safety Network later expanded the definition of harm prevention to include “the freedom from accidental or preventable injuries caused by medical care” (AHRQ PSNet, n.d.). Although the definition is not yet complete (Mitchell, 2008), patient safety practices have been defined as “those that reduce the risk of adverse events related to medical care exposure in a variety of diagnoses or conditions.”
Mitchell (2008) states that the origins of the patient safety problem are classified in terms of type (error), communication (e.g., failures between professionals or between patient and professional, and between professionals and non-medical staff), patient management (e.g., inadequate delegation, failure to follow up, incorrect referral, or misuse of resources), and clinical performance (before, during, and after the intervention).
Strategies to prevent patient safety errors and improve healthcare processes (Hughes, 2008) include the use of simulators, bar codes, and computerized entry via clinical applications, as well as team resource management. Communication is an effective way to improve patient safety, especially if it’s assertive, clear, and positive (Belim & Vaz de Almeida, 2017).
Discussion and results
These reflections resulted from a qualitative study with Portuguese nurses (n = 30) who participated in five focus groups from August to October 2019 and from five in-depth interviews with health literacy specialists. The focus groups and interviews were assessed separately and then combined and compared. Thematic analysis is a very useful approach for producing quality analyses (WHO, 2019).
As mentioned in the focus groups, with qualitative content analysis, patient support has to be given in stages, and the health professional must always confirm that the patient has acknowledged and understood the information. In an in-depth interview, an organ transplant coordinator (a medical doctor) at a large reference hospital in the greater Lisbon area of Portugal said that sometimes, doctors think certain words or phrases are understandable but the family does not actually comprehend them. These include “the patient is in a stable situation,” where the family thinks the patient is about to be in good health, or “the patient has kidney failure,” where the family simply does not understand what “kidney failure” means.
Any care transition, whether to a different unit in the hospital, to a separate hospital, or to the patient’s home, increases risk. Communication between the team and the patient or family should be a factor to consider in risk consequences. In addition to written information, the health professionals in the focus groups said that communication must be accurately and intelligibly conveyed to the patient and family, because certain communications are very difficult to understand.
Focus group participants, especially those in physical medicine and rehabilitation, stressed the importance of talking clearly, assertively, and respectfully to patients and families. The components of the healthcare professional’s verbal and nonverbal language may be innate, but according to focus group participants, professionals “need to be learned and trained to produce even more effective patient outcomes, especially given the critical need for their understanding and safety in action.” Harmony and reciprocity between the patient and professional allows communication that flows easily and is mutually understandable.
Focus groups also noted the need for patient training to be an active partnership. Empowerment as a way to promote commitment is an established concept for healthcare. In this clinical and communicative process, an overview of the patient is helpful and promotes better results.
The health professional should be an “observer” reporting on the rehabilitation health professionals participating in the focus group. In this domain, the professional should get used to looking at patients in their physiological, psychological, social, and cultural dimensions.
Cultural beliefs can also be a barrier to real commitment and involvement from both patients and practitioners. One such barrier is the hierarchical tradition, based on clinicians’ training as figures of power and authority. The focus groups confirmed that this hegemony of physicians still exists in some organizations, even between doctors and nurses, contributing to poor communication as a reflection of patient safety “when teams do not understand each other.” Ricciardi & Shofer (2019) stress that these more hegemonic styles can lead to a dictatorial style of management, which in turn can lead to inefficient and insecure teamwork.
We must also mention the spread of universal precautions in health literacy. These precautions aim to simplify communication and confirm patient understanding, thereby minimizing miscommunication; easing navigation in the consultation environment and the health system; and supporting patients’ efforts to improve their health.
With these points on attitude and safety behaviors in mind, we can reflect on the ongoing need for open dialogue with the patient through assertive behavior and communication, clear language, and positive action where partnership, reciprocity, and a holistic vision of a true health professional “observer” are always present to improve health outcomes.
Cristina Vaz de Almeida is director of Post Graduate Course on Health Literacy at ISPA in Portugal; she is also a PhD student in communication science and health literacy at ISCSP.
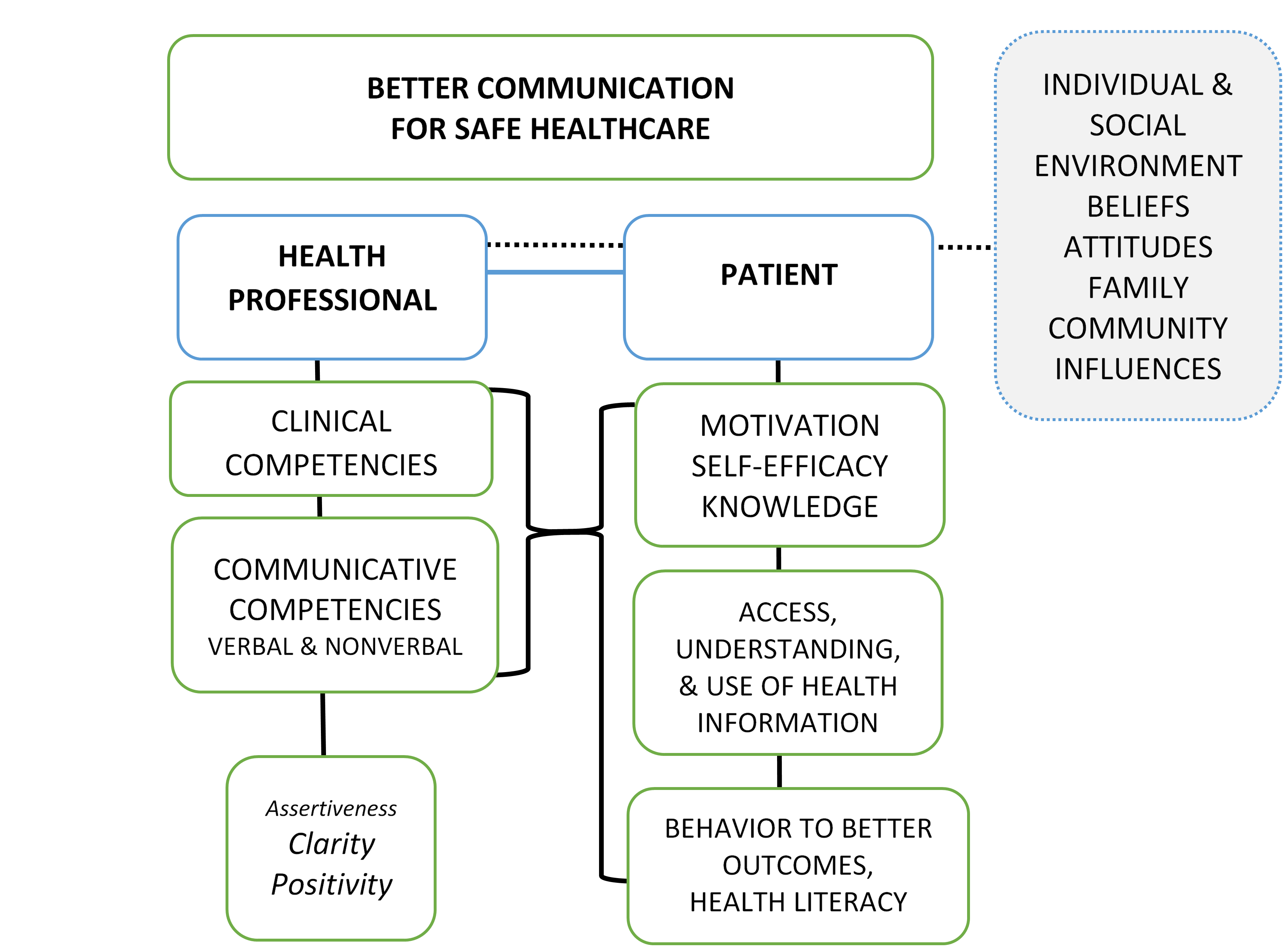
Figure 1: Communication for Better Health Literacy and Health Outcomes
References
AHRQ PSNet. (2019, June). Tips & tools: Questions are the answer. Retrieved from https://www.ahrq.gov/patients-consumers/patient-involvement/ask-your-doctor/tips-and-tools/index.html
AHRQ PSNet. (n.d.). Patient safety. Retrieved from https://psnet.ahrq.gov/glossary/p
Aspden, P., Corrigan, J., Wolcott, J., & Erickson, S. M. (Eds.). (2004). Patient safety: Achieving a new standard for care. Washington, DC: National Academies Press.
Belim, C., & Vaz de Almeida, C. (2017). Healthy thanks to communication: A model of communication competences to optimize health literacy: Assertiveness, clear language, and positivity. In V. E. Papalois & M. Theodospoulous (Eds.), Optimizing health literacy for improved clinical practices (pp. 124–152). Hershey, PA: IGI Global.
Brega, A. G., Barnard, J., Mabachi, N. M., Weiss, B. D., DeWalt, D. A., Brach, C., … West, D. R. (2015). AHRQ health literacy universal precautions toolkit (2nd ed.). Retrieved from https://www.ahrq.gov/health-literacy/quality-resources/tools/literacy-toolkit/healthlittoolkit2.html
Egener, B., & Cole-Kelly, K. (2004). Satisfying the patient, but failing the test. Academic Medicine, 79(6), 508–510.
Hughes, R. G. (Ed.) (2008). Patient safety and quality: An evidence-based handbook for nurses. Rockville, MD: Agency for Healthcare Research and Quality.
Mitchell, P. H., Heinrich, J., Moritz, P., & Hinshaw, A. S. (1997). Outcome measures and care delivery systems: Introduction and purposes of conference. Medical Care, 35(11 Suppl), NS1–5.
Mitchell, P. H. (2008). Defining patient safety and quality care. In Hughes, R. G. (Ed.), Patient safety and quality: An evidence-based handbook for nurses (Chapter 1). Rockville, MD: Agency for Healthcare Research and Quality.
Ricciardi, R., & Shofer, M. (2019). Nurses and patients: Natural partners to advance patient safety. Journal of Nursing Care Quality, 34(1), 1–3. https://doi.org/10.1097/ncq.0000000000000377
WHO. (2019). Improving health through health literacy. Public Health Panorama, 5(2–3), 123–329.
