Patient Engagement in Patient Safety: Barriers and Facilitators
March / April 2010
![]()
Patient Engagement in Patient Safety:
Barriers and Facilitators
Patient safety has been at the forefront of recent domestic and international policy initiatives. The release of the Institute of Medicine’s (IOM) 2000 report To Err Is Human solidified the patient safety movement and the role that leadership and knowledge can play in preventing adverse events from occurring. Using information from two studies conducted in the United States in 1984 and 1992, the IOM estimated that between 44,000 and 98,000 people die annually from medical errors, with approximately 7,000 of these deaths resulting from medication errors (Kohn et al., 2000). In Canada, the seminal Canadian Adverse Events Study (Baker et al., 2004) shed light on the magnitude of medical and medicine errors within that country’s healthcare system. In fact, the overall incidence rate of adverse events in Canada in 2000 was 7.5%, representing 185,000 adverse events annually (Baker et al., 2004). Astonishingly, 70,000 of these adverse events were also found to be potentially preventable.
As a result of these findings, many patient safety strategies within hospital settings have focused on such as patient identification, surgical site identification, wound management, continuity of care, sound-alike drug names, drug labelling and storage, and allergy identification. (Cook, Render & Woods, 2000; Nolan, 2000; Burke, 2003). Furthermore, patient safety strategies have been focused mainly on error-prevention from a healthcare provider and systems perspective. This has led to increased education and awareness of patient safety issues within the workplace and targeting technologies as a means to reduce human error. While addressing these technical and complex issues is essential in reducing the number of adverse events experienced, recent studies and campaigns have begun to target the patient as an integral team member in the reduction of medical errors. Campaigns such as the World Health Organization’s (WHO) Patients for Patient Safety have begun to highlight the role that patients can play in improving the safety and quality of care received, including being knowledgeable about their treatment plans and asking healthcare professionals for clarification when they don’t understand. Understanding the role of patients in patient safety as well as the barriers and facilitators to engaging patients in patient safety practices will help reduce adverse events.
Patient Engagement in Patient Safety
Patient engagement in patient safety is aimed at increasing the awareness and participation of patients in error-prevention strategies. To better understand how to effectively engage patients in error prevention strategies, we conducted a literature review of Canadian and international articles and studies on patient engagement, patient safety, and safety culture. This resulted in a proposed framework for patient engagement in patient safety (Figure 1). The following sections will explore these barriers and facilitators in more depth and assess their effectiveness on shifting patient perceptions and behaviors. Barriers and facilitators are summarized in Tables 1 and 2, respectively.
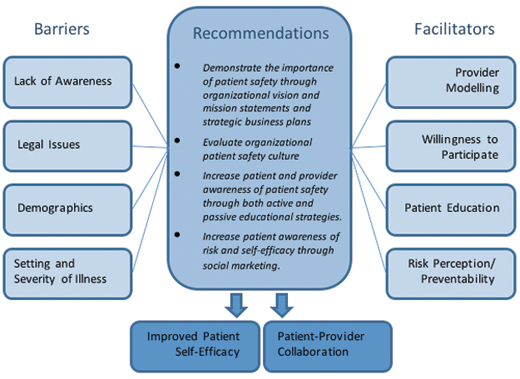
Figure 1. Proposed framework for patient engagement in patient safety
| Barrier | Description |
| Awareness |
|
| Traditional Patient/Provider Roles |
|
| Self-Efficacy |
|
| Healthcare Setting and Illness |
|
| Demographics |
|
| Legality |
|
Table 1. Barriers to patient engagement in patient safety practices.
| Facilitator | Description |
| Provider Modelling |
|
| Perception of Risk and Preventability |
|
| Willingness to Participate |
|
Table 2. Facilitators of patient engagement in patient safety
Barriers
Awareness
The most commonly cited barrier to patient engagement in patient safety practices is an individual’s lack of awareness and understanding of what patient safety is. In fact, in one survey of patients in the United States, the term “patient safety” was actually viewed as less important than the term “medical errors,” suggesting that patients do not understand that patient safety and medical errors commonly refer to the same topic (Hibbard, Peters & Tusler, 2005). Interestingly, the convenience sample within this study contained a large percentage of university graduates (55.4%), suggesting that even educated individuals may be unaware of the term and concept of patient safety. While patient safety is an often used and understood term between healthcare professionals, we believe that to obtain maximal impact of patient safety issues within the public, it may be more appropriate to frame the concept around medical errors as this is typically taken more seriously by patients. However, the study also showed that increased education surrounding patient safety did mitigate this confusion.
To capitalize on a greater knowledge of patient safety and ensure engagement of patients in error prevention strategies, many experts purport that education must occur before the provider encounter. Brennan and Safran (2004) suggest that public awareness of safety issues could be increased through public education and public negotiation of safety goals. Peters et al. (2006) suggest that patient safety awareness might be best achieved through an increased perception of risk and preventability. Specifically, if patients are not aware that medical or medicine errors constitute a risk for them while receiving treatment, then patient engagement is unlikely to occur. Moreover, if there is a perception of risk, but patients do not feel like their actions can prevent errors from occurring, patients will be unlikely to become active participants in error prevention strategies (Peters et al., 2006). Patients must also be aware of the proper reporting mechanisms for when errors do occur and understand what steps they can take to address medical errors within the public sphere (Brennan and Safran, 2004).
Traditional Patient and Provider Roles
The traditional patient-provider relationship has also been identified as an impediment to greater patient participation in patient safety. Three major patient safety studies in the United States (Marella et al., 2007; Waterman et al., 2005; Davis et al., 2008) identified that patients feel less comfortable asking direct and confrontational questions of their providers, such as, “Did you wash your hands?” or asking if the physician could mark their surgical site. Davis et al. (2008) also found that patients are less willing to adhere to patient safety practices that they view as challenging to the healthcare staff’s clinical abilities. This was somewhat mitigated by the healthcare professional’s designation, with more individuals willing to ask challenging questions of nurses than of physicians. Waterman et al. (2005) reported similar results with only 45.5% of the respondents indicating that they would feel comfortable asking medical personnel whether they had washed their hands. Even more shocking was the fact that only 4.5% of respondents actually did ask their care provider if they had washed their hands, indicating a large discrepancy between feeling comfortable to perform an error prevention action and actually performing that action. The traditional patient-physician relationship, in which the physician is perceived to have more knowledge about individual health concerns, is an impediment to patients asking questions of their physician, even if they feel that that their safety might be compromised and that they could play a role in preventing an error. This disconnect might point to broader cultural issues.
Self-Efficacy
Self-efficacy refers to the ability of patients to perceive themselves as playing an important role in error prevention. Essentially, it measures whether or not they view their participation in patient safety as being efficacious. Hibbard et al. (2005) asked respondents, “How much can you rely on your own knowledge and alertness to protect yourself from medical errors?” with a possible range of 0 (not at all) to 6 (can rely a lot). Results indicated that the majority of respondents had moderate self-efficacy and that this was related to the presence of family members in the hospital and having previously read about medical errors. Moderate to high perceived health efficacy was strongly related to the likelihood of taking error prevention actions and was also found to be related to the likelihood of taking unfamiliar prevention actions and questioning healthcare workers about washing their hands. However, 21% of respondents indicated that they had low self-efficacy for error prevention This is a substantial hurdle to involving patients in patient safety and needs to be addressed through further education and awareness. However, with little research and data on how effective patient engagement in patient safety is or could be, patients may continue to view their involvement as mere lip service.
Healthcare Setting and Illness
The healthcare setting and nature of illness can in and of itself prevent some patients from engaging in error prevention strategies. A critical literature review conducted by Davis et al. (2007) found that patients are more comfortable communicating with their family physician than with hospital staff, which might impede increased participation of patients within the hospital setting. While this information is discouraging in that many preventable medical and medicine errors happen in hospital and post-discharge, it does signal that increased educational opportunities within the primary care setting might exist. In addition to feeling uncomfortable, hospital settings present a number of other difficulties to engaging patients, particularly with critically ill patients and those admitted to the emergency department. Waterman et al. (2006) found that patients who were critically ill lacked the capacity to fully involve themselves in error prevention even if they had wanted to do so. To date, it has also been difficult to involve critically ill patients in patient engagement studies, so there is not a great deal of information available about patient representatives as a means of greater patient involvement in patient safety. The emergency room setting also presents a number of obstacles for involving patients. Emergency patients are often unaware of their healthcare problem, and this may create difficulties when asking patients to participate in decision processes and also discourages patients from speaking up (Davis et al. 2007).
Demographics
Patient demographics have been shown to have some impact on the likelihood of patient involvement in error prevention strategies. In a survey of 2,078 hospitalized patients discharged from 11 Midwest hospitals in the United States, Waterman et al. (2006) found that older patients and Caucasians were less likely to ask the purpose of a medication when compared to other groups. Davis et al. (2007) found that, in general, younger patients want to be involved more than older patients. On average, however, older patients have more complex and chronic health issues and are on a greater number of medications, suggesting that for this demographic, greater awareness and education of patient safety issues may be necessary. Also, the use of patient representatives or proxies may help ensure that older patients are involved in their treatment. Other study results cited in Davis et al. (2007) stated that women wanted more involvement than men and that highly educated patients opted for a more active role in the quality of their care.
Legality
The expectation that patients will become increasingly involved in their own care and error prevention has come with some uncertainty how this may change the responsibility of both provider and patient. Critics of increased patient involvement in patient safety have cited that it is unreasonable to expect patients to assume more responsibility for their health when they are already in the vulnerable position of being ill. Lyons (2007) argues that if patients are entrusted with the task of ensuring their safety, then physicians may rely too heavily on this, leading to a reduction of safeguards on the physician side. Liability for medical and medicine errors could also be called into question. However, it is important to note that patient engagement in patient safety practices is not intended to enforce a standard on patients; rather, it is to encourage patients who are interested and willing to become more involved in their care and to become better educated about potential risks. Nonetheless, it will be necessary to ensure that the scope of patient engagement is well defined and that neither the legal responsibilities of physicians are reduced nor that patient responsibility is increased.
Facilitators
Provider Modelling
One of the most commonly cited facilitators of patient engagement in patient safety is provider behavior or physician modelling. Patients are less likely to engage in behavior that they perceive to be confrontational or challenging. Davis et al. (2007) found that when patients were instructed by a doctor to ask challenging questions of themselves and nurses, patient willingness to ask was significantly increased. Thus, physician instruction and education surrounding the reasons why patients should ask questions may have a significant impact on patient error prevention behaviors. Waterman et al. (2006) found similar results with their survey and suggest physician modelling as an integral part of patient education of patient safety practices. The authors propose that patient safety programs should target patient fears about challenging and insulting their healthcare provider by posting education material in hospital and waiting rooms encouraging patients to ask questions or having providers wear reminder buttons that encourage patients to ask them if they’ve washed their hands (Waterman et al., 2006). Fundamentally, provider modelling and education surrounding the acceptability of asking healthcare providers questions should ultimately lead to greater patient comfort in engaging in these behaviors. Hibbard et al. (2005) also suggest that training patients to be more assertive in their encounters with healthcare providers may lead to greater involvement in error prevention behaviors, as it has previously been shown to enhance patient involvement in their own care and improve care outcomes.
Perception of Risk and Preventability
One of the greatest barriers to patient involvement in patient safety is patient awareness of the potential risks of encountering the healthcare system; if patients do not feel that they are at risk for a medical or medication error, they are unlikely to take preventative actions. Furthermore, even if patients are aware of risks, they might not be able to determine if or when an error occurs. A survey conducted in the United States found that although patients were aware of medical errors, they were unable to determine if they had in fact received proper treatment, making it impossible to identify potential errors (VHA, 2000). When patients understand the consequences of errors, they experience heightened perception of risk and worry, and the timing of those perceptions is predictable and manageable (Peters et al., 2006). Essentially, medical errors must be perceived by the public as real and definable risks and must be viewed as preventable through engagement in patient safety practices. Hibbard et al. (2006) build upon the concept of perceived preventability by arguing that patients must perceive their actions as being effective in preventing errors from occurring. In order to increase this feeling of effectiveness, the authors suggest exposing patients to specific information about errors and how error prevention can mitigate these risks.
Willingness to Participate
Patient safety surveys have shown that patients are generally interested in engaging in error prevention strategies. Waterman et al. (2006) found that, on the whole, most respondents felt very comfortable engaging in patient safety practice, and 98% agreed that hospitals should educate patients about error prevention. Marella et al. (2007) also found that patients were overall inclined to engage in patient safety practices, particularly when it involved gaining additional information about their health and treatment. Certain subpopulations of patients, such as those with chronic diseases and those who are terminally ill, may also be more inclined to engage in error prevention strategies. Davis et al. (2007) argue that willingness to participate might correlate to the progression of a patient’s disease and that different motivations might emerge over time. Tapping into this willingness to participate and ensuring appropriate education opportunities for all patients can help to encourage participation in patient safety practices.
The Role of Organizational Culture
The role of organizational culture in the adoption and dissemination of patient safety practices has been examined increasingly in the past few years. The role of a “safety culture” is well documented in other high-risk sectors, such as the airline industry, but is a relatively new approach in healthcare. Nieva and Sorra (2009) describe safety culture within healthcare as a “…performance shaping factor that guides the many discretionary behaviours of healthcare professionals toward viewing patient safety as one of their highest priorities.” Essentially, a safety culture acknowledges that errors will occur and strives to identify and reduce potential risks. Creating a culture that is aware of patient safety risks, supportive of employees, and values leadership accountability is vital to ensuring that patient safety practices are effectively incorporated throughout a healthcare organization. A major component of provider uptake of patient safety and error prevention is the creation of an atmosphere of trust and openness. When healthcare providers are worried about the ramifications of error reporting, or feel that such reporting would tarnish their reputations, then there is a decreased likelihood they will speak up when an error or near miss occurs—making it impossible for the organization to learn and develop safer practices. Furthermore, healthcare professionals may be less willing to share information with patients when an error or near miss has occurred.
Assessing the safety culture of an organization is the first step to introducing cultural change (Nieva and Sorra, 2009). Safety culture assessment tools seek to examine the values, behaviors, and perceptions of organizational members to better understand the organizational culture and capacity for adoption of safety practices. The most effective tools survey both frontline staff and administrators to better understand the cohesiveness of culture and to determine whether there are major discrepancies between the vision of the organization and the actual adoption of safety practices by frontline staff.
Assessment tools can also be used as part of a broader adherence to continuous quality improvement (CQI) by completing the tool annually, comparing results, and enhancing organizational learning. Continual cultural assessments are vital in ensuring a consistent and continuing patient safety culture within a healthcare organization. Interestingly, assessing the patient safety culture of an organization inherently raises staff awareness of patient safety issues and practices, whether intended or not (Nieva and Sorra, 2003). The initiation of patient safety cultural assessments can signal to organizational members that patient safety is a strategic priority for the organization. Thus, safety culture assessments are an ideal first step in raising organizational awareness of potential issues and creating a shared understanding of changes to take place.
Conclusions
Examining the barriers and facilitators to patient engagement in patient safety leads to a number of conclusions. Firstly, a significant disconnect exists between the willingness of patients to engage in patient safety practices and their actual likelihood to take action. Within a healthcare organization, changes in organizational and professional cultures may help improve patient comfort levels and involvement in patient safety practices. The adoption of a safety culture can enhance patient engagement through increased provider modelling, patient education, and enhanced awareness. Patient self-efficacy should be enhanced through increased patient education and greater transparency of medical and medication errors. Increasing patient knowledge that risks exist and that many errors are preventable could greatly improve patient participation in patient safety practices. Recommendations for greater patient engagement in patient safety are provided in Figure 1. Fundamentally, healthcare organizations should strive to facilitate greater patient involvement in patient safety practices through the identification, assessment, and elimination of potential barriers and the adoption of a proactive safety culture.
Andrea Scobie is currently pursuing an interdisciplinary PhD at Dalhousie University, exploring the roles of perception and organizational culture in engaging patients in patient safety and error prevention strategies. Her other research interests include quality of care, healthcare delivery, and primary care reform. Scobie may be contacted at andrea.scobie@dal.ca
D. David Persaud is a professor in the School of Health Administration at Dalhousie University and is cross-appointed to the Department of Ophthalmology. His research interests are focused in two areas: The first is as a member of a multi-disciplinary team involved in the development of integrated systems of vision care. The second area of research is the utilization of performance management systems to enhance organizational learning and change.
References
