The Silent Treatment: Why Safety Tools and Checklists Aren’t Enough
September/October 2011
The Silent Treatment: Why Safety Tools and Checklists Aren’t Enough
Poor communication is deadly, especially in critical care settings (Wachter, 2010; The Joint Commission, 2010). When communication breaks down in intensive care units (ICU) and operating rooms, the result is catastrophic harm (Alvarez, 2006; Gandhi, 2005) and even death (Consumers Union, 2009; Institute of Medicine, 2000). The Silent Treatment study, conducted in 2010 by the American Association of Critical-Care Nurses (AACN), the Association of periOperative Registered Nurses (AORN), and VitalSmarts, examines an especially dangerous kind of communication breakdown: risks that are known, but not discussed, or “undiscussables.”
|
The Magnet Recognition Program, a program of the American Nurses Credentialing Center, recognizes healthcare organizations that provide nursing excellence. It is based on more than a dozen quality indicators and standards of nursing practice as defined in the third edition of ANA Nursing Administration: Scope & Standards of Practice (2009). The Beacon Award for Excellence, a program of the American Association of Critical-Care Nurses, recognizes excellence at the unit level where patients receive their principal nursing care after hospital admission. It is based on criteria in six categories: leadership structures and systems; appropriate staffing and staff engagement; effective communication, knowledge management and best practices; evidence-based practices and processes; and patient outcomes. |
The study builds on findings from research conducted in 2005 by AACN and VitalSmarts (Maxfield et al., 2005) as documented in the article Silence Kills: The Seven Crucial Conversations for Healthcare. Silence Kills identified seven concerns that often go undiscussed and contribute to avoidable medical errors. It linked the ability of health professionals to discuss emotionally and politically risky topics in a healthcare setting to key results like patient safety, quality of care, and nursing turnover, among others.
The Silent Treatment shows how nurses’ failure to speak up when risks are known undermines the effectiveness of current safety tools. It then focuses on three specific concerns that often result in a decision to not speak up: dangerous shortcuts, incompetence, and disrespect. The Silent Treatment tracks the frequency and impact of these communication breakdowns, then uses a blend of quantitative and qualitative data to determine actions that individuals and organizations can take to resolve avoidable breakdowns.
Background
When communication breaks down, it breaks down into two categories: honest mistakes and undiscussables (Argyris, 1980). Honest mistakes include accidental or unintentional slips and errors—for example: poor handwriting, confusing labels, difficult accents, competing tasks, language barriers, distractions, etc.
An undiscussable is not a slip or error; it’s a calculated decision to avoid or back down from the conversation.
Information-based solutions like protocols, checklists, and systems don’t do much to solve the breakdowns in this second category. The literature on organizational silence (Morrison et al., 2000; Detert, 2007) suggests that solving undiscussables will require deeper changes to cultural practices, social norms, and personal skills.
Safety Tools and Organizational Silence—Story Collector Findings
Rich, qualitative data was gathered via a Story Collector, which was completed by 2,383 registered nurses, of whom 169 were managers. The Story Collector listed four survey safety tools that are intended to prevent unintentional slips and errors (Universal protocol checklist, WHO checklist, SBAR handoff protocol, and drug-interaction warning systems). The respondents (nurses) were then asked how often they had been in situations where one of these tools worked—where it warned them of a problem that otherwise might have been missed and harmed a patient:
- 85% of the nurses said that a safety tool had warned them of a problem the team might have otherwise missed at least once.
- 29% said they were in this situation at least a few times a month.
These results strongly confirm that safety tools work. Operating rooms and ICUs are fast paced, complex, and full of disruptions. Checklists, protocols, and warning systems are an essential guard against unintentional slips and errors.
However, the Story Collector data documented that the effectiveness of these safety tools is being undercut by undiscussables:
- 58% of the nurses said they had been in situations where it was either unsafe to speak up or they were unable to get others to listen.
- 17% said they were in this situation at least a few times a month.
Three Undisscussables: Traditional Survey Findings
Quantitative data was gathered via a Traditional Survey, which was completed by 4,235 nurses, of whom 832 were managers. The Traditional Survey examined three of the seven concerns found in the 2005 study—dangerous shortcuts, incompetence, and disrespect. These concerns are not necessarily prompted by any of the safety tools examined with the Story Collector. Instead, they tend to emerge over time, as people observe each other on the job. Findings from non-supervisory nurses who completed the current study’s Traditional Survey are summarized below:
Dangerous shortcuts
- 84% of respondents say 10% or more of their colleagues take dangerous shortcuts.
- Of those people, 26% say these shortcuts actually harmed patients.
- Despite these risks, only 31% shared their full concerns with the person.
Incompetence
- 82% say 10% or more of their colleagues are missing basic skills.
- 19% say they have seen harm come to patients as a result of incompetence.
- Only 21%, however, spoke to the incompetent colleague and shared their full concerns.
Disrespect
- 85% of respondents say 10% or more of the people they work with are disrespectful and therefore undermine their ability to share concerns or speak up about problems.
- And yet, only 24% confronted their disrespectful colleagues and shared their full concerns.
The data presents a convincing case. Organizational silence leads to communication breakdowns that harm patients:
- More than four out of five nurses have concerns about dangerous shortcuts, incompetence, and disrespect.
- More than half say shortcuts have led to near misses or harm.
- More than a third say incompetence has led to near misses or harm.
- More than half say disrespect has prevented them from getting others to listen to or respect their professional opinion.
- Fewer than half have spoken to their managers about the person who concerns them the most.
- And fewer than a third have spoken up and shared their full concerns with the person who concerns them the most.
The data also show that nurses are more likely to take their concerns to their managers than they are to speak directly to the person they are concerned about. Since working through the hierarchy is often assumed to be the appropriate way to address a problem, it is important to examine how well this strategy works.
Results from Nurse Managers
The responses from the 832 nurse managers who completed the Traditional Survey were reviewed separately from the non-supervisory nurses. A surprising finding was that managers do not appear to be a reliable path for resolving concerns about dangerous shortcuts, incompetence, or disrespect.
- 41% of the nurse managers reported that they spoke up to the person whose dangerous shortcuts create the most danger for patients.
- Only 28% spoke up to the person whose missing competencies created the most danger for patients.
- Only 35% spoke up to the person whose disrespect had the greatest negative impact.
This study shows that taking problems to a manager, and assuming he or she will handle them, doesn’t produce the kind of immediate and reliable results needed in healthcare.
Resolving Organizational Silence—What Organizations Can Do
Undiscussables represent an entrenched organizational problem. As such, they will require a multifaceted solution (Kotter et al., 1979; Maxfield et al., 2011). A helpful way to think about this multifaceted solution is to use six sources of behavioral influence (Patterson et al., 2008) as summarized in the VitalSmarts Influencer model below:
Source 1—Personal Motivation. If it were up to them, would the nurses want to speak up? Does it feel like a moral obligation or an unpleasant annoyance to them?
Source 2—Personal Ability. Do the nurses have the knowledge and skills they need to handle the toughest challenges of speaking up?
Source 3—Social Motivation. Are the people around them (physicians, managers, and co-workers) encouraging them to speak up when they have concerns? Are the people they respect modeling speaking up?
Source 4—Social Ability. Do others step in to help them when they try to speak up? Do others support them afterward so the risk doesn’t turn against them? Do those around them offer coaching and advice for handling the conversation in an effective way?
Source 5—Structural Motivation. Does the organization reward people who speak up or does it punish them? Is speaking up included in performance reviews? Are managers held accountable for influencing these behaviors?
Source 6—Structural Ability. Does the organization establish times, places, and tools that make it easy to speak up—for example, surgical pauses, SBAR handoffs, etc.? Are there times and places when caregivers are encouraged to speak up? Does the organization measure the frequency with which people are holding or not holding these conversations—and use these measures to keep management focused on this aspect of patient safety?
Organizations must overwhelm the problem of organizational silence. This requires deploying multiple sources of influence—all aimed at motivating and enabling people to speak up. Research shows that combining four or more of sources of influence can increase success by as much as ten times (Grenny, et al., 2008).
The Magnet Recognition Program® and the AACN Beacon Award for ExcellenceTM are two national programs that encourage a multifaceted approach to improving patient care.
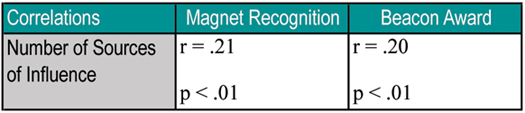
Although neither program specifically targets all six sources of influence, each requires that a broad range of strategies be employed in combination. The positive correlations in the table below show that hospitals that achieve Magnet Recognition or AACN’s Beacon Award use significantly greater numbers of the six sources of influence (Table 1).
Table 1. Correlations from Magnet Recognition and AACN Beacon Award
The negative correlations shown in Table 2 demonstrate that these multifaceted approaches are associated with fewer concerns, less patient harm, and lower intent to leave the organization or profession. While many of the correlations are significant, the associations aren’t as consistent or as strong as those found with the number of sources of influence.
Table 2. Further Correlations from Magnet Recognition and AACN Beacon Award
Recommendations
The results presented in The Silent Treatment point the way toward positive change. Below are recommendations for how healthcare organizations can use this multifaceted approach to create a safety culture where people speak up effectively when they have concerns.
Establish a design team.
Enlist a small team that includes senior leaders, managers in the targeted areas, and opinion leaders among physicians, nurses, and other caregivers. This design team works with all caregivers to identify crucial moments, vital behaviors, and strategies within each of the six sources of influence described below. The design team then provides a few initial strategies within each of the six sources and helps teams in patient care areas select, modify, and create additional strategies.
Identify crucial moments.
There are a handful of perfect-storm moments when circumstances, people, and activities combine to put safety protocols at risk. The design team needs to identify and spotlight these crucial moments so that people will recognize them. An example of one of these crucial moments is when the surgery schedule is pushed into the evening, and people are in a rush.
Define vital behaviors.
People need to know what to say and do when they find themselves in these crucial moments. These are the vital behaviors that keep patients safe. Following are examples of vital behaviors used at Spectrum Health, the largest not-for-profit health care system in West Michigan. Spectrum Health worked with Vital-Smarts to create vital behaviors and a six-source influence plan which, took them from a hand hygiene rate hovering just above the national average of 60% to 97%.
- 200% accountability. Each staff member is 100% accountable for following safe practices and 100% accountable for making sure others follow safe practices.
- Thank you. Staff members make it safe for others to hold them accountable. When they are reminded of a safety practice, they thank the other person and redouble their efforts to keep the patient safe.
Develop a playbook.
Safety requires that the vital behaviors be acted on in a highly reliable way—especially during the crucial moments when they are the toughest. The most powerful way to make sure these behaviors are consistently followed is to create a multifaceted influence plan that uses all six sources of influence. This plan is captured in a playbook that can be disseminated throughout the organization.
The recommendations above are a starting point. The goal is to create a playbook that includes crucial moments, vital behaviors, and strategies within each of the six sources of influence. Organizations and teams can then use the ideas within the playbook to create a multifaceted plan that is tailored to their individual situation.
Conclusions
The Silent Treatment details the success and limitations of current safety tools. Most of these tools work by warning caregivers of potential problems. But warnings only create safety when the caregiver who is warned is able to speak up and get others to act. The data in this study reveal that caregivers, including nurse managers, are often unable to accomplish this level of candor. They fail to have an influence and patients are harmed.
Key programs such as the Magnet Recognition Program and AACN’s Beacon Award for Excellence have contributed to progress in this area, most likely because they demand that organizations take a multifaceted approach to improving care. AORN provides powerful tools—one focused on Just Cultures and another on Human Factors—that can help organizations create a culture of safety. This research shows that explicitly multifaceted approaches, such as the six sources of influence contained in the VitalSmarts Influencer model, are the most predictive of success.
Healthcare organizations need to learn from both successful individuals and successful organizations. The communication skills that exceptional nurses already have should become the norm among all caregivers. Healthcare organizations should establish a design team, identify crucial moments, define vital behaviors, and develop a playbook that combines change strategies within each of the six sources of influence.
Together, these approaches will create a safety culture where people who know of or strongly suspect risks do speak up, even when they encounter resistance. Patients can no longer afford to have issues related to their health and safety remain undiscussable.
David Maxfield is the vice president of research for VitalSmarts, where he leads a series of consulting and research projects on the role influence plays in initiating and sustaining organizational change. He is also the coauthor of The New York Times bestsellers Influencer and Change Anything. Maxfield did his doctoral work in psychology at Stanford University. He can be contacted at maxfield@vitalsmarts.com.
Joseph Grenny is the cofounder of VitalSmarts, an innovator in evidence-based corporate training and organizational performance. His solutions have helped 300 of the Fortune 500 enable lasting behavior change and achieve dramatic results. Grenny is also the coauthor of four New York Times bestsellers: Crucial Conversations, Crucial Confrontations, Influencer, and Change Anything. He can be contacted at grenny@vitalsmarts.com.
Ramón Lavandero is the director of communications & strategic alliances for the American Association of Critical-Care Nurses and clinical associate professor at Yale University School of Nursing. Lavandero received a master’s degree in nursing from Yale University. A fellow of the American Academy of Nursing, he was the first nurse to participate in the Hispanic Leadership Fellows program. He can be contacted at ramon@aacn.org.
Linda Groah has been the CEO and executive director of the Association of periOperative Registered Nurses since March 2007. Throughout her career, Groah has focused on improving patient safety. She has introduced several patient safety initiatives including the “Just Culture” concept, which is now a national healthcare standard. She can be contacted at gdavis@aorn.org.
For more information visit the Silent Treatment study website: www.silenttreatmentstudy.com.
References