NEWS
New Coalition Brings Attention, Action to Address Errors in Diagnosis
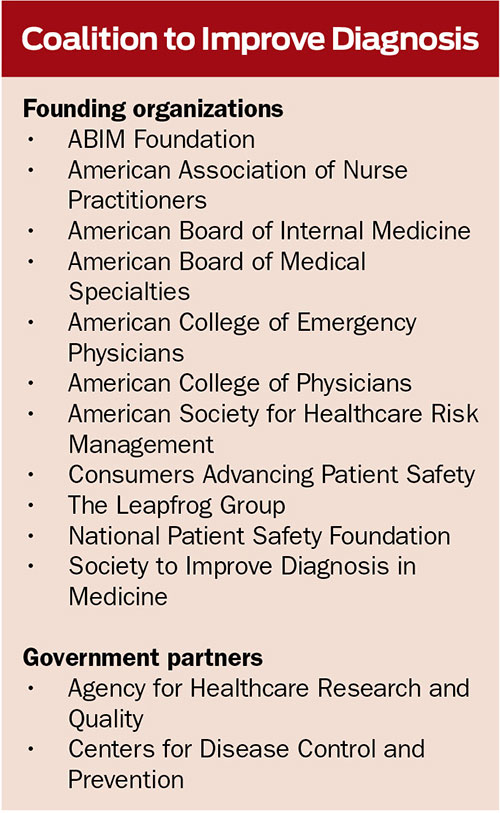 More than a dozen major medical societies and healthcare organizations, including patient and consumer advocates and government partners, have joined forces to address diagnostic errors in medicine through the newly formed Coalition to Improve Diagnosis.
More than a dozen major medical societies and healthcare organizations, including patient and consumer advocates and government partners, have joined forces to address diagnostic errors in medicine through the newly formed Coalition to Improve Diagnosis.
The Society to Improve Diagnosis in Medicine (SIDM) established and will lead the Coalition. The Coalition’s founding member organizations represent clinicians and other healthcare professionals as well as patients and families, employers, consumer advocates, researchers, policymakers, and educators.
Shared principles
The shared principles of the Coalition have been approved unanimously by the member organizations and represent their shared beliefs about diagnostic error as well as their commitment to addressing it as a systemwide issue in healthcare:
- A timely, accurate, and efficient diagnosis is appropriately the expectation of every patient.
- Diagnosis, which by its very nature involves uncertainty, is one of the most difficult and complex tasks in healthcare, involving both human and systematic elements, and it is made more difficult by an explosive growth in knowledge and tools that are both helpful and problematic.
- The overwhelming majority of diagnoses are accurate, but the burden to patients, families, healthcare professionals, and society associated with diagnostic error is significant.
- Every participant in healthcare, from providers and the extended team of healthcare professionals, to patients and families, and to others who are key to the success of our healthcare system, including industry, payers, researchers, educators and more, has a role to play in reducing the burden.
- The organizations that comprise the Coalition to Improve Diagnosis believe that they must and will individually and collectively take action to help solve this problem.
For more information about the Coalition, including membership, visit www.improvediagnosis.org/CID.
Patient Blood Management: Patient Safety Implications
While blood has played a central role in clinical practice for decades, the proof of blood transfusion safety and efficacy remains ill defined compared to other forms of medical and surgical intervention. Over the last 50 years, researchers have accumulated a great deal of data regarding the risks associated with the practice. In fact, research suggests that more restrictive transfusion strategies are safe for most patient populations.
Healthcare saw an increase in demand for blood products starting in the 1980s, due in part to the greater complexity of surgical procedures and the use of more aggressive treatment regimens for cancer (Thomson et al., 2009). Recent data indicate that blood use is decreasing (U.S. HHS, 2013), but some experts predict that demographic factors, such as the aging population, may increase transfusions in the near future.
The National Patient Safety Foundation (NPSF) recently released an educational module about patient blood management (PBM). PBM is the scientific use of safe and effective medical and surgical techniques designed to minimize and manage anemia and decrease bleeding. It focuses on multidisciplinary and multimodality preventive measures to decrease the need for blood transfusions and ultimately improve clinical patient outcomes.
A combination of a monograph and video lectures, the five-part NPSF module allows learners to go at their own pace. NPSF is also planning to offer a free educational webcast on PBM this fall. For more information, visit www.npsf.org.
References:
Thomson, A., Farmer, S., Hofmann, A., Isbister, J. P., & Shander, A. (2009). Patient blood management – A new paradigm for transfusion medicine? ISBT Science Series, 4, 423-435.
U.S. Department of Health and Human Services (U.S. HHS). (2013). The 2011 National Blood Collection and Utilization Survey report. Retrieved from http://www.hhs.gov/ash/bloodsafety/2011-nbcus.pdf.
ANA Sets ‘Zero Tolerance’ Policy for Workplace Violence, Bullying
The nursing profession “will no longer tolerate violence of any kind from any source,” the American Nurses Association (ANA) declared in a new position statement on violence in healthcare workplaces released in August.
“Taking this clear and strong position is critical to ensure the safety of patients, nurses, and other healthcare workers,” said ANA President Pamela F. Cipriano, PhD, RN, NEA-BC, FAAN. “Enduring physical or verbal abuse must no longer be accepted as part of a nurse’s job.”
ANA’s position statement, developed by a panel of registered nurses (RN) representing clinicians, executives, and educators, addresses a continuum of harmful workplace actions and inactions ranging from incivility to bullying and physical violence. The statement defines bullying as “repeated, unwanted harmful actions intended to humiliate, offend, and cause distress,” such as hostile remarks, verbal attacks, threats, intimidation, and withholding support.
The statement calls on RNs and employers to share responsibility in creating a culture of respect and implementing evidence-based strategies to prevent workplace violence. It cites research showing that some form of incivility, bullying, or violence affects every nursing specialty, occurs in virtually every practice and academic setting, and extends into all educational and organizational levels of the nursing profession.
A recent ANA survey of 3,765 RNs found that nearly one-quarter of respondents had been physically assaulted while at work by a patient or a patient’s family member, and up to half had been bullied in some manner, either by a peer (50%) or a person in a higher level of authority (42%).
The position statement’s recommendations to prevent and mitigate violence, in addition to setting a “zero tolerance” policy, include:
- Establishing a shared and sustained commitment by nurses and their employers to a safe and trustworthy environment that promotes respect and dignity
- Encouraging employees to report incidents of violence, and never blaming employees for violence perpetrated by non-employees
- Encouraging RNs to participate in educational programs, learn organizational policies and procedures, and use situational awareness to anticipate the potential for violence
- Developing a comprehensive violence prevention program aligned with federal health and safety guidelines, with RNs’ input
To prevent bullying, the ANA encourages RNs to commit to “promoting healthy interpersonal relationships” and become “cognizant of their own interactions, including actions taken and not taken.” Among recommendations for employers are to:
- Provide a mechanism for RNs to seek support when feeling threatened
- Inform employees about available strategies for conflict resolution and respectful communication
- Offer education sessions on incivility and bullying, including prevention strategies
To view the position statement and other resources, including ANA’s booklet, Bullying in the Workplace: Reversing a Culture, and toolkits from other organizations, visit www.nursingworld.org/Bullying-Workplace-Violence.
