Reducing the Noise: Improving Actionable Alerts
By Joshua M. Schmees, PharmD; and Maggie Wong, PharmD, BCPS
In 2012 when Hospital Sisters Health System (HSHS), a 14-hospital system in Illinois and Wisconsin, started using computerized provider order entry (CPOE), physicians were overwhelmed by the number of alerts they got from the ordering system. Though the alerts were meant to prevent errors, the barrage simply wore the physicians down, often to the point of ignoring some warnings altogether.
We needed to find a way to address this perplexing alert fatigue problem and increase alert utilization to improve patient care. Our goal was to make interactions with the system more meaningful for our physicians. To accomplish this, we set out to find a way to adjust alerts to a level that optimally leverages clinical decision support at the point of care and minimizes alert fatigue.
Studying the situation
To get a better handle on the alert fatigue issue, we reviewed published literature, looking for situations and institutions similar to our own. In particular, a meta-analysis of 17 studies on CPOE environments showed that alert override rates varied from 49% to 96% and that 2.3% to 6% of the overridden alerts resulted in adverse drug events (van der Sijs et al., 2006).
We were determined to reduce alert fatigue at HSHS. We knew that if we didn’t, alert-burdened physicians would continue to dismiss some warnings that were significant. At the same time, we had to avoid eliminating effective alerts that provide important information.
Improving quality & safety
A quality care improvement program implemented throughout HSHS focused on enhancing patient safety by reducing alert fatigue and improving clinical decision support by increasing alert specificity, avoiding inappropriate alerts, clarifying information, and improving usability. To kick off the alert fatigue reduction initiative, pharmacy staff members identified alert override patterns, looking for potential changes that could reduce alert fatigue and lead to the adoption of more meaningful alerts.
Drug-drug interaction alerts bubbled to the top of the remediation list; many of them lack specificity and data necessary for developing clear action steps. In addition, drug-drug interactions are often influenced by multiple variables and may warrant additional fine-tuning.
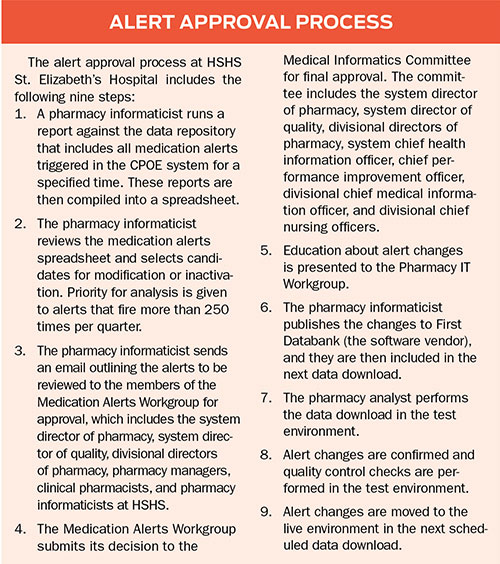
As pharmacy informaticists, we were able to identify ineffective alerts, but reducing them required collaboration with other clinicians. Therefore, we had to put processes in place that made it possible for a Medication Alerts Workgroup to evaluate each alert. With this group of clinical experts, the scope of our analysis expanded to include alerts for drug allergies, dose range, and duplicate therapies.
To aid in this collaborative process, we started using software that allows us to keep track of customizations, create an audit record, and load the results of modifications directly into the decision support system for immediate use in the workflow. As the hospital implemented this alert management tool, the workgroup realized that a comprehensive alert approval process was in order (see sidebar).
Realizing results at HSHS St. Elizabeth’s Hospital
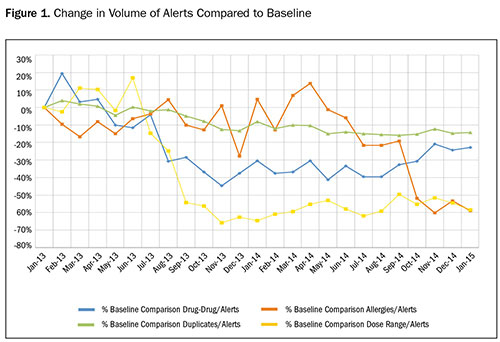
With this medication alert solution and process in place, we have successfully reduced alert fatigue at HSHS. For example, at one facility in the system, St. Elizabeth’s Hospital in Belleville, Illinois, between January 2013 and April 2015, we made improvements in the following categories:
- Alerts related to drug-drug interactions have been reduced 21.78%, from 2,211 to 1,892
- Dose-range checking alerts fell 60.66%, from 927 to 299
- Alerts associated with drug allergies dropped 61.42%, from 462 to 195
- Duplicate alerts were reduced 21.05%, from 15,494 to 13,383
Reducing alert fatigue, however, is just one element of success; we are also improving clinical decision support by offering more meaningful alerts. The ratio of interventions to alerts—the number of actions taken (orders replaced and erased) relative to all alerts received in CPOE—increased from 12.4% in December 2013 to 16.7% in December 2014 and has at times been as high as 18%. As a result of increasing the intervention to alert ratio, the remaining alerts enabled physicians to catch 215 more potential medication errors in December 2014 than in December 2013.
Physicians are receiving alerts that are more meaningful and valuable. To maintain this level of improved patient safety, we monitor the system for effects caused by changing alert settings. For example, the number of overridden alerts for drug-drug interactions increased in September when a drug-drug interaction severity level was increased, a connection we might not have made without continuous monitoring.
With better clinical decision support, physicians are now able to focus on relevant alerts, as shown with the improvement in alerts addressed. In addition, because physicians spend less time with unnecessary overrides, HSHS can move forward with implementing other types of customized clinical decision support. Addressing the issues and impacts of alert fatigue has benefited HSHS’ implementation of CPOE and improved patient safety.
Joshua Schmees is system pharmacist of informatics and automation services at HSHS in Belleville, Illinois. He received his Doctor of Pharmacy degree from Ohio Northern University Raabe College of Pharmacy in 2009. Prior to joining HSHS, Schmees served as the HSHS St. Elizabeth’s Hospital pharmacy manager of operations and technology. Schmees currently serves as a preceptor for the Southern Illinois University Edwardsville School of Pharmacy, a first-year post-graduate preceptor for pharmacy residents at HSHS St. Elizabeth’s Hospital, and the second-year post-graduate pharmacy residency program director for pharmacy informatics. Schmees may be contacted at Joshua.Schmees@hshs.org.
Maggie Wong is a pharmacy informaticist with HSHS. She received her doctor of pharmacy degree from Midwestern University Chicago College of Pharmacy in 2013. Prior to joining HSHS, Wong served as the HSHS St. Elizabeth’s Hospital PGY-1 pharmacy resident and HSHS Southern Illinois Division PGY-2 pharmacy informatics resident. At HSHS, Wong currently serves as the first-year post-graduate preceptor for pharmacy residents at HSHS St. Elizabeth’s Hospital. Wong may be contacted at Maggie.Wong@hshs.org.
References:
van der Sijs, H., Aarts, J., Vulto, A., et al. (2006). Overriding of drug safety alerts in computerized physician order entry. Journal of the American Medical Informatics Association, 13(2), 138-147.
