Lessons Learned: Implementing a Digital Process for Informed Consent
By Samia Zia and Nneka C. Egbuniwe
The modern concept of informed consent was born barely a century ago in Schloendorff v. Society of New York Hospital—a 1914 case establishing that procedures performed on a person without the patient’s explicit permission are a form of battery. The notion that risks and alternatives must be disclosed to a patient was established in 1957 in Salgo v. Leland Stanford Jr. University Board of Trustees. That idea was further refined in 1972 in Canterbury v. Spence to specify that the risks disclosed should include those that a reasonable patient might want to know.
Today, the requirements for informed consent are spelled out in statute and case law in all 50 states. Typically, states fall into one of two major groups when it comes to how much information should be disclosed to patients as part of the informed consent process (Select state law provisions, n.d.; Studdert et al., 2007):
- Professional standard: Roughly 23 states, including New York and Florida, require that patients be presented with the information that would be communicated by other physicians with similar background and experience and practicing within their community
- Patient standard: Another approximately 23 states, including Ohio and Texas, require that patients be presented with the information that a reasonable or prudent patient would want to know in order to make a decision about a treatment or procedure
A handful of states employ laws that blend aspects of the patient and professional standards, resulting in a “hybrid” standard for disclosure. In all cases, however, informed consent involves much more than merely signing a document. When done properly, it is a conversation between provider and patient that is documented in a consistent manner as part of the medical record.
One health system’s approach
At Parkland Hospital in Dallas, this philosophy for patient-provider conversations helped drive a recent initiative to automate the documentation of the informed consent process, as well as facilitate that process through integration with the electronic health record (EHR). Although many providers have moved to an EHR, a large number continue to use paper forms to obtain consent. This manual process can create patient s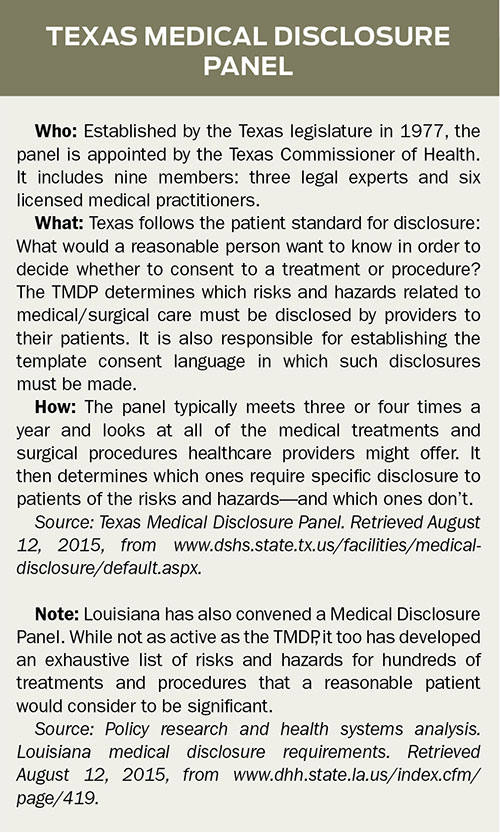 afety issues if information is missing, such as the procedure description or surgical site, and is called for during the pre-procedure verification or during the timeout. A paper-based consent process also impacts provider productivity if forms are lost or misplaced at the time of surgery, thereby delaying the start of a case.
afety issues if information is missing, such as the procedure description or surgical site, and is called for during the pre-procedure verification or during the timeout. A paper-based consent process also impacts provider productivity if forms are lost or misplaced at the time of surgery, thereby delaying the start of a case.
Consequently, at the teaching hospital and main campus of the Parkland Health and Hospital System, the organization saw an opportunity to circumvent potential patient safety risks, ease provider workflows, and ensure regulatory compliance.
Texas mandate governs disclosures
The content of informed consent discussions by providers in Texas, including Parkland, is subject to a unique regulatory oversight body called the Texas Medical Disclosure Panel (TMDP) (see sidebar). This state-mandated, nine-member committee of medical and legal experts reviews medical and surgical procedures to determine:
- Which risks and hazards must be disclosed to patients
- The content of the disclosures
- The form in which the disclosures must occur
The TMDP standardizes and periodically updates two lists—one for procedures requiring full disclosure of specific risks and hazards, and another for those requiring no specific disclosure. Even in the latter case, providers in states with a patient standard still have a duty to disclose all risks or hazards that could influence a reasonable person in deciding to consent to a procedure. (In Texas, this duty was clarified in a 1983 Texas Supreme Court case, Peterson v. Shields, 652 S.W.2d 929, 931.)
In addition to improving patient education and safety, complying with the regulation gives providers a degree of protection against legal liability. Providers who comply with the TMDP rules are more easily protected from claims that they failed to adequately disclose risks.
As one of the country’s largest public and academic teaching hospital systems with more than a million patient visits annually, Parkland clearly expended enormous resources to supply the numerous and highly detailed, procedure-specific consents to patients in paper form. At the same time, ensuring that those consents reflected the latest versions of the so-called “Texas risks” was a very time-intensive and manual process.
Seeking to simplify
Parkland desired a comprehensive means to not only manage the regulatory disclosure requirements of the “Texas risks,” but also to improve accuracy, consistency, and productivity related to informed patient consent. The hospital wanted to reinforce consent as a discussion between patient and provider, rather than just the completion of documents.
Leaders realized that their paper-based system was time-consuming and not particularly provider- or patient-friendly. Furthermore, the hospital didn’t want administrative resources to promote a “faux” paperless system that required printing out paper forms to obtain signatures, then scanning the completed documents back into the EHR. Instead, the hospital looked for a way to simplify the entire consent process by automating the forms—which would stay current with TMDP updates—and immediately incorporating signed documents into the electronic record.
To ease provider workflows, Parkland also sought a tool that would launch natively within the organization’s EHR, without a separate login or password. Consent forms would be automatically populated with the appropriate patient and procedure information, and digital images would be saved to the patient’s EHR as soon as they were complete.
Automating consent: Five tips for success
- First and foremost, Parkland understood that any informed consent application should enhance communication between provider and patient—not complicate it. So the development and implementation team at Parkland recommends these five tips to support technical execution and provider adoption of automated consent:
- Involve the experts from the beginning. A cross-sectional group of key stakeholders should help assess automated informed consent technologies and how they support the overall patient workflow. This group might include representatives from health information management, operational excellence, information technology, legal, regulatory, performance improvement, patient safety and quality, direct patient care, nursing leadership, and medical staff. Mapping out patient consent workflows up front is one way to ease integration with the EHR.
- Define any specific conditions. Every organization has its “non-negotiables” that must be applied when evaluating potential technology solutions. For example, Parkland required its automated consent application to launch through its existing EHR to make it easier and faster for providers to use, which in turn helped improve physician acceptance.
- Identify a pilot area. Use a pilot program to test the concept, identify best practices, and allow for adaptations to ensure achievement when the tool is ready for hospital- or systemwide rollout. Keep in mind that a pilot program does not need to be based on specialty or size. In Parkland’s case, an initial rollout in the urology clinic was based on the clinic’s volume, its predictable environment, and its willingness to embrace change—which made it easier to work through all of the hiccups expected during a pilot launch. A second pilot in emergency general surgery was conducted prior to the “big bang” organizational implementation. Emergency general surgery was chosen because it interacts with all the main areas where consents are obtained (ER, OR, inpatient units, and outpatient clinics). Midlevel providers in the department who trained as “super users” became particularly capable champions; they proved instrumental in the pilot’s success due to their ability to relate with physicians and other providers.
- Consider the patient experience. Beyond supporting providers, think about how automating the informed consent process can aid in patient satisfaction. For instance, many patients complain when providers have to look away or turn their backs to enter information into an EHR. So, to ease the patient-provider conversation, Parkland’s new process allows providers to quickly search for the proper consent form, complete the required fields, and have the form ready before entering the patient’s room. This allows the provider to spend more bedside time interacting with the patient and less time searching for content or completing form fields. Even something as simple as attaching the signature capture device to a clipboard so that it’s easier for the patient to hold and use has also positively impacted the patient experience.
- Plan for glitches. Anticipate changes of all types, from content to connectivity. For example, since the Parkland facility was built in 1954, its construction was not conducive to wireless data transfer. This meant that the tablets the hospital wanted to use as electronic signature capture devices did not always reliably connect to the EHR. One solution, before the hospital moved into a brand-new 862-bed, 17-story facility in August 2015, was to use bedside workstations and mobile computers instead.
While some physicians may be reluctant to give up paper consent forms, Parkland’s team of providers embraced the change and reached 72% utilization of the automated solution just one month after go-live. Without a doubt, the transition was bolstered by the early involvement of physicians and nurses, in addition to well-defined testing. The strong adoption rate demonstrates the importance of making the electronic informed consent process a seamless, user-friendly component of the EHR.
Develop a disclosure strategy
Only Texas and Louisiana provide procedure-specific guidance on what risks to disclose to patients. Meanwhile, the CMS interpretive guidelines for risk disclosure (2015)—guidelines that apply to all states—echo the professional standard by citing practitioner judgment while also noting that the risks disclosed should include those material to the patient:
Material risks could include risks with a high degree of likelihood but a low degree of severity, as well as those with a very low degree of likelihood but high degree of severity. Hospitals are free to delegate to the responsible practitioner, who uses the available clinical evidence as informed by the practitioner’s professional judgment, the determination of which material risks, benefits and alternatives will be discussed with the patient.
Consequently, healthcare organizations should review the disclosure requirements set forth in their states with their preferred legal counsel and risk management personnel. If a state employs the patient standard for disclosure, the risks and potential complications disclosed for complex procedures may be quite lengthy. Most organizations will additionally find it useful to standardize the risks presented to different patients for the same procedure—regardless of which standard the state employs. Last, the application of technology to assist with standardization, and with documentation of the informed consent process, may also be effective.
The authors work at Parkland Health & Hospital System in Dallas.
Samia Zia is a senior project manager for quality, safety, and performance improvement.
Nneka Egbuniwe is the deputy general counsel responsible for supporting operations and regulatory compliance.
References:
Canterbury v. Spence, 464 F.2d 772 (D.C. Cir. 1972).
Centers for Medicare & Medicaid Services. (2015, July 10). State operations manual. Appendix A: Survey protocol, regulations and interpretive guidelines for hospitals. §482.24(c)(4)(v). Retrieved August 19, 2015, from www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/som107ap_a_hospitals.pdf.
Salgo v. Leland Stanford Jr. University Board of Trustees, 154 Cal App2d 560, 317 P2d 170 (1957).
Schloendorff v. Society of New York Hospital, 211 N.Y. 125, 105 N.E. 92 (1914).
Select state law provisions regarding disclosure requirements. (n.d.). Retrieved July 6, 2015, from http://healthcare.uslegal.com/informed-consent/select-state-law-provisions-regarding-disclosure-requirements/.
Studdert, D. M., Mello, M. M., Levy, M. K., Gruen, R. L., Dunn, E. J., Orav, E. J., & Brennan, T. A. (2007). Geographic variation in informed consent law: Two standards for disclosure of treatment risks. Journal of Empirical Legal Studies, 4(1), 103-124.
