Viewpoint: Emerging Challenges for Patient Safety – Opportunities for Our Finest Hours
Emerging Challenges for Patient Safety: Opportunities for Our Finest Hours
By Daniel L. Cohen, MD, FRCPCH, FAAP
The birth of the patient safety movement can be linked intimately to Lucian Leape’s seminal article Error in Medicine (1994), published six years before the Institute of Medicine’s report To Err is Human (2000). Since that time, much has been accomplished in the field of patient safety, but frankly not enough. We have much more to do to decrease morbidity and mortality, and the terrain is about to become even more challenging.
Though some real improvements in safety have been achieved, millions of patients are harmed and thousands still die every year as a result of the healthcare services they have received in hospitals and other settings. Benevolent though our intentions may be, many of our practices and processes are not safe, our hospitals are not safe, and, sadly, we are not safe. Current estimates are that more than 150,000 people die annually from healthcare. Although that number is somewhat debatable, sufficient evidence supports estimates near this figure (Leape, 1994; Institute of Medicine, 2000)—three to four baseball stadiums full of mothers, fathers, and children die every year.
As challenging as things are today, I am becoming increasingly concerned that we have not devoted sufficient time toward anticipating future challenges. In fact, the greatest threat to patient safety may well be the steady deterioration in health of the U.S. population related to obesity and the range of co-morbid illnesses that are due to, or walk hand-in-hand with, obesity. We are confronting a tsunami in illness burden and coincident requirements for healthcare services, in excess of current levels. This may substantially impair our ability to be safe and will likely put severe pressure on our healthcare financing and payment infrastructure (Cawley & Meyerhoefer, 2012). This tsunami is not below the horizon by any means; the waves are already lapping at our shores, and our feet are already wet.
The solutions to current and future challenges confronting patient safety will not only include transforming healthcare (Leape et al., 2009), but also will include improving health and reversing the progressively evolving overweight and obesity endemic.
Achievements to Date
Much has been accomplished to improve safety through the standardization of processes, the development and implementation of checklists and care bundles, and through team training that harkens to the aviation model of crew resource management (Rebmann & Greene, 2010; Marra et al., 2011; Pronovost et al., 2006; Berenholtz et al., 2004; Dodek et al., 2004; Weaver et al., 2014). However, even when evidence-based checklists are adopted or adapted, it appears that there are non-believers and non-adherers in our midst (Lambert et al., 2013). Many are aware of the recent controversy regarding the evidence supporting the use of the WHO Safe Surgery Checklist (Haynes et al., 2009; Urbach et al., 2014; Leape, 2014). Strict adherence and meaningful implementation seems to be the key to sustained improvements. Consistently demonstrating broad improvements across a large, very complex, and disjointed healthcare system remains difficult (Landrigan et al., 2010).
In addition, we are struggling to overcome errors in diagnosis and therapeutics that confound us daily. Practicing medicine is not simply about utilizing checklists. Many human factors liabilities interfere with our ability to arrive at correct diagnoses in a timely fashion. The processes of diagnosis and clinical reasoning are complex (Leape, 1994; Groopman, 2007), and busy clinicians often utilize short-cuts, fall victim to psychological biases, overly rely on technologies that lead to false conclusions and increase the costs of healthcare without benefiting patients, and/or come to conclusions before sufficient and reliable evidence is available to confirm working diagnoses.
Not only are the processes of diagnosis complex but providing therapeutics, whether behavioral, medical or surgical, also presents challenges as overutilization of technologies is common and often associated with harm. Best outcomes from procedures are neither assured nor consistent.
Furthermore, everyone involved in healthcare understands that the successful implementation of therapeutic plans requires thoughtful engagement with patients who, for the large proportion of healthcare services, are the ones who actually execute our care plans, for better or worse. We cannot and will not improve patient safety unless we engage with our patients as partners, working equally toward achieving optimal healthcare outcomes.
In the high-reliability industry paradigm, engagement with front-line stakeholders is crucial to safety (Weick & Sutcliffe, 2001). In healthcare, the clinicians and the patients are the front-line experts who must be engaged for success. Furthermore, these stakeholders need to respect and value each other. The most notable example of failures in this model can be found when one examines readmissions within 30 days. It has been estimated that upwards of 50 percent of readmissions may be due to failures in successfully implementing care plans, and each of these failures is a patient safety incident where someone has been harmed, money has been spent, and limited resources were utilized on readmissions, to the detriment of our system (Van Walraven et al., 2011).
Finally, when one examines the impact of hospital culture on patient safety, at least as far as one can ascertain by surveys, the results again are disappointing. Though many hospitals will tout the improvements in culture over time, the fact is that very large gaps remain across the board in terms of governance, leadership, followership, and staff engagement, even though incident reporting may be increased (Weingart et al., 2004). Incident reporting, and more importantly, proactive risk identification are the soil upon which process improvements can be built and must be sustained.
As Leape et al point out, what is needed is a major transformation in healthcare (2009). We absolutely must improve our transparency. We must improve our care integration. We must restore joy and meaning in our work. We must robustly engage with patients as partners in healthcare, we must reform medical education, and we must reinvigorate and sustain our focus on what matters most to patients.
The question is, will this be enough and will we accomplish this soon enough?
 The Terrain is Changing
The Terrain is Changing
If the demographics of the health of the population were to remain stable, then one might accurately create models that would be reasonably predictive of the kinds and burdens of illnesses likely to come through the doors of outpatient settings and hospitals over time. These predictions then could be adjusted based upon regional population growth and social demographics that might be unique to specific ethnic groups. Unfortunately, the health of our population is not stable. In fact, the health of the population across ethnic groups is deteriorating (Ward et al., 2013). This may well accelerate and complicate projections for healthcare utilization and adversely impact our ability to provide safe, reliable, and equitable care.
Obesity is the Challenge!
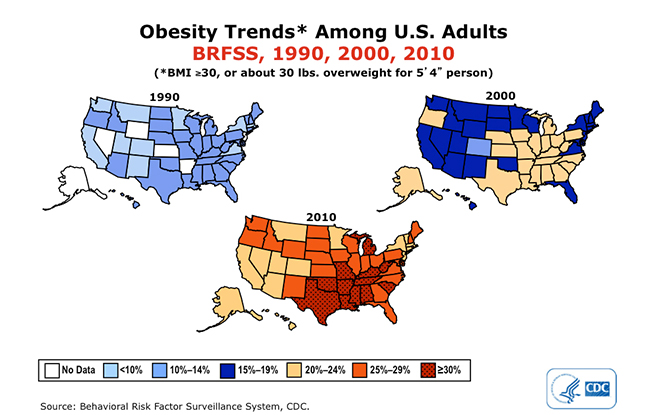
We are about to be overwhelmed by an endemic of obesity. Obesity is associated with and/or a causal factor for metabolic syndrome (hypertension, hyperglycemia, abdominal fat preponderance, and hyperlipidemia), type 2 diabetes, cancers (endometrial, breast, colon, prostate), coronary heart disease, stroke, non-alcoholic fatty liver disease, gallbladder disease, sleep apnea, osteoarthritis, gynecological problems (including polycystic ovarian syndrome) and mental health disorders (Department of Health and Human Services). The maps shown above portray the increasing prevalence of obesity in the United States, and there are now estimates that by 2030 approximately 50 percent of the adult population in the United States will be obese (BMI =/>30) (Finkelstein, et al., 2012). Another substantial proportion on top of this will be overweight (BMI =/>25) and well on the road to obesity.
Meeting the Challenge
The progressively worsening obesity endemic presents real challenges and will affect our ability to provide safe care and to transform our healthcare system. Dr. Robert Lustig, a prominent endocrinologist who has written widely on obesity and the sugar addiction cycle, has commented that confronting obesity is not simply a matter of altering behavior. Individuals who are obese are biochemically and physiologically different than the non-obese. Altered biochemistry and physiology will substantially undermine behavior modification efforts every time. Considerable evidence shows that obesity now begins in utero as obese young women, living in an environment of hyperinsulinemia, are giving birth to infants, who although not necessarily obese at birth, may be destined to become obese as their fat cells accumulate lipid very early in life (Lustig, 2013; Lustig, 2011).
Obesity has become the new normal for many segments of our population. Obese individuals often have obese friends and relatives (Christakis & Fowler, 2007). A recent survey of obese children revealed that many of these do not perceive themselves as being obese (Sarafrazi et al., 2014).
This is not to say that we should not adopt/adapt the traditional behavioral modification approaches of encouraging exercise and dieting to reduce weight in those already affected, but rather that this will be very difficult to accomplish for an individual, let alone an entire population. Safe and effective medications, behavior modification, and commitments to change lifestyle may work, but more important is the need to take on the commercial food industry, which has to some extent seduced and manipulated our population incredibly effectively over the past several decades (Harris et al., 2009). Primarily, to impact the future, we must attack the obesity endemic at the prevention level because for far too many, the die has already been cast.
Thus, looking toward the horizon, improving patient safety must be linked intimately to improving the health of the population. If we do not accomplish this, we are in real trouble. We must transform our thinking about health in order to transform our projections for healthcare utilization and for patient safety. What happens inside our offices and hospitals is a reflection of the nature, burden, and severity of illnesses with which our patients present, and these are likely to get a lot worse before they get better.
Conclusions
Addressing the future complexities and challenges that are portrayed in this article will require concerted efforts by clinicians partnering with patients to improve their health so that, together, we can reverse the obesity endemic and chronic illness burden. Many will look to healthcare professionals to solve the obesity problem, but healthcare can only be a small part of the solution.
Obesity is really society’s problem, and all elements of society, in the broader sense, must work to solve the problem collectively — sociologically, educationally, politically, and economically. Society must provide an environment where availability of affordable healthy food options is the norm, not the exception, and where meaningful incentives and opportunities for healthful living are provided. A variety of financial incentive-based programs have recently been developed and are now being utilized by major healthcare payers that can result in substantial savings on health insurance costs for participants now available through provisions of the Affordable Care Act.
Transforming the ways we provide healthcare will be an important part of the solution. For healthcare professionals, the future population health challenges that obesity and increasing chronic disease burden entail should be viewed as unique opportunities for patient safety’s finest hours.
Daniel Cohen is international medical director for Datix, a prominent clinical risk management software company. He was formerly chief medical officer for the U.S. Department of Defense TRICARE Healthplan covering over 9,000,000 beneficiaries. In this capacity he had oversight for clinical quality and patient safety across this complex system. Cohen trained in pediatrics and hematology/oncology at the Boston Medical Center (Boston University) and the Children’s Hospital and Dana Farber Cancer Institute (Harvard University). He is a senior fellow of the Royal College of Paediatrics and Child Health (UK) and a fellow of the American Academy of Pediatrics. Cohen may be contacted at dcohen@datix.co.uk.
The views expressed in this article are those of the author and do not necessarily reflect the official policy or position of the U.S. government, the U.S. Department of Defense, or the Uniformed Services University of the Health Sciences.
Cohen D. L. (2014). Emerging challenges for patient safety: Opportunities for our finest hours. [Viewpoint]. Patient Safety & Quality Healthcare, 11(6), 20–24.
References
Berenholtz, S., Pronovost, P., Lipsett, P., et al. (2004). Eliminating catheter-related bloodstream infections in the intensive care unit. Critical Care Medicine, 32, 2014 –20.
Cawley, J., & Meyerhoefer C. (2012). The medical care costs of obesity: an instrumental variables approach. Journal of Health Economics, 31, 219-30.
Christakis, N., & Fowler, J. (2007). The spread of obesity in a large social network over 32 years. New England Journal of Medicine, 357, 370-79.
Department of Health and Human Services. Agency for Healthcare Quality and Research. Overweight and obesity, causes and consequences. Retrieved July 30, 2014, from http://www.cdc.gov/obesity/adult/causes/index.html
Dodek, P., Keenan, S., Cook, D., et al. (2004). Evidence-based clinical practice guideline for the prevention of ventilator-associated pneumonia. Annals of Internal Medicine, 141, 305-13.
Finkelstein, E., Khavjou, O,. Thompson, H., et al. (2012). Obesity and severe obesity forecasts through 2030. American Journal of Preventive Medicine, 42, 563-70.
Groopman, J. (2007). How doctors think. New York: Houghton Mifflin Company.
Harris, J., Pomeranz, J., et al. (2009). A crisis in the marketplace: How food marketing contributes to childhood obesity and what can be done. Annual Review of Public Health 30, 211-225.
Haynes, A., Weiser, T., Berry, W., et al. (2009). A surgical safety checklist to reduce morbidity and mortality in a global population. New England Journal of Medicine, 360, 491-9.
Institute of Medicine. Committee on Quality of Health Care in America. (2000). To err is human: Building a safer health system. Washington, DC: The National Academy Press.
Lambert, M., , Palomar, M., Agodi A., et al. (2013). Prevention of ventilator-associated pneumonia in intensive care units: an international online survey. Antimicrobial Resistance and Infection Control, 2, 1-8.
Landrigan, C., Parry, G., Bones, C., et al. (2010). Temporal trends in rates of patient harm resulting from medical care. New England Journal of Medicine, 363, 2124-34.
Leape, L. (1994). Error in medicine. Journal of the American Medical Association, 272, 1851-57.
Leape, L., Berwick, D., Clancy, C., et al. (2009). Transforming healthcare: a safety imperative. Quality & Safety in Health Care, 18, 424-28.
Leape, L. (2014). The checklist conundrum. New England Journal of Medicine, 370, 1063-64.
Lustig, R. (2013). The Complete Skinny on Obesity (Video file). Retrieved from http://youtu.be/moQZd1-BC0Y.
Lustig, R. (2011). Obesity: nature or nurture? Obesity before birth. Berlin: Springer Science and Business Media, LLC.
Marra, R., Camargo, T., Goncalves, P., et al. (2011). Preventing catheter-associated urinary tract infection in the zero-tolerance era. American Journal of Infection Control, 39, 817–22.
Pronovost, P., Needham, D., Berenholtz, S., et al. (2006). An intervention to decrease catheter-related bloodstream infections in the ICU. New England Journal of Medicine, 355, 2725-32.
Rebmann, T., Greene, L. (2010). Preventing catheter-associated urinary tract infections: An executive summary of the Association for Professionals in Infection Control and Epidemiology, Inc, Elimination Guide. American Journal of Infection Control, 38, 644-46.
Sarafrazi, N., Hughes, J., Borrud, L., et al. (2014). Perception of weight status in U.S. children and adolescents aged 8–15 years, 2005–2012. National Center for Health Statistics, NCHC Data Brief, #158, 1-8.
Urbach, D., Govindarajan, A., Saskin, R., et al. (2014). Introduction of surgical safety checklists in Ontario, Canada. New England Journal of Medicine, 370, 1029-38.
Van Walraven C., et al. (2011). Proportion of hospital readmissions deemed avoidable: A systematic review. Canadian Medical Association Journal, 183, E391-E402.
Ward, B., Schiller, J,. et al. (2013). Prevalence of multiple chronic conditions among US adults: estimates from the National Health Interview Survey, 2010. Preventing Chronic Disease 10:120203. DOI: http://dx.doi.org/10.5888/pcd10.120203
Weaver, S., Dy, S., & Rosen, M. (2014). Team-training in healthcare:a narrative synthesis of the literature. BMJ Quality and Safety, 23, 359-372.
Weick K., & Sutcliffe, K. (2001). Managing the unexpected: assuring high performance in an age of complexity. San Francisco: Jossey-Bass.
Weingart, S., Farbstein, K., Davis, R., et al. (2004). Using a multihospital survey to examine the safety culture. Joint Commission on Quality and Patient Safety, 30, 125-32.
