A New Approach to Fall Prevention in Inpatient Care
A New Approach to Fall Prevention in Inpatient Care
Implementing Remote Audiovisual Monitoring of At-Risk Patients
By Jane McCurley, RN, DNP, MBA; and James Pittman, RN, MSN
Like most hospitals, our organization—St. David’s North Austin Medical Center in Texas—is focused on preventing patient falls. The Agency for Healthcare Research and Quality estimates that 700,000 to 1 million patients fall in U.S. hospitals each year. At least 30% of falls result in moderate to severe injury, and each year 11,000 inpatients die as a result (Boushon et al., 2012). Falls in the hospital setting increase overall healthcare costs and increase the liability of the organization where the fall occurred. An inpatient fall is also considered a hospital-acquired condition (HAC); as such, none of the care linked to the fall is reimbursed by Medicare and other payers. Falls with serious injury cost
hospitals an average of more than $28,000 to treat, adding more than six days to the average length of stay (CMS, 2008).
In 2005, The Joint Commission introduced a National Patient Safety Goal aimed at reducing falls with an associated injury. Since then, hospitals have been intently focused on reducing falls. From 2005 to 2010, a study of the University HealthSystem Consortium Patient Safety Net database demonstrated a 27% reduction of falls with injury and a 34% reduction in falls requiring life sustaining intervention (Williams et al., 2014). Though those data demonstrate progress in reducing falls with injury, a significant opportunity for further prevention remains.
St. David’s North Austin Medical Center (SDNAMC) is a 332-bed, community-based hospital. In 2012, 2013, and 2014 our facility was designated a Top 100 Hospital by Truven Analytics. Additionally, our organization was a finalist for the Malcolm Baldrige award both in 2013 and 2014. Prevention of falls is a major focus for our organization.
With an understanding that fall prevention is multifactorial and requires a comprehensive approach to successfully decrease the occurrence, SDNAMC has deployed many strategies to reduce falls. Our Falls Committee reviews incidents and looks for causes and patterns. It seeks out best practices within the parent HCA system and provides toolkits and resources on falls and falls prevention. We have implemented fall-risk assessment screenings, physical sitters, improved staff communication, a variety of motion-sensitive alarms, no-slip socks, special door signage, and other tactics. Some of these interventions have proven effective.
Patients presenting with altered mental status are often at risk for falling. Providing a physical sitter is a common approach to prevent falls with injury for this population. Though this is likely the most aggressive (and resource intensive) fall prevention strategy available, it is also the most effective. A physical sitter provides constant patient surveillance and is able to redirect a confused, forgetful patient or, if needed, physically assist the patient to prevent a potential fall. With an aging baby boomer population and increased patient acuity index, the demand for physical sitters occurs at varying rates. Utilizing physical sitters, though often requisite to provide safe patient care, is not without cost or burdensome impact.
Physical sitters increase care delivery costs and/or redirect available resources. At SDNAMC, staff are often reassigned as physical sitters. For example, a 32-bed inpatient unit typically has two patient care technicians (PCTs) assigned to 16 beds to assist the nursing care provided on the unit. When the need for a physical sitter develops, attempts to call in additional staff to cover the shift are made. Often, the need is unable to be covered, so one of the two PCTs will be assigned as a sitter, creating a 16-bed PCT support void that is divided among the remaining PCT and nurses.
In an effort to find a solution to these issues, one of the authors, Jane McCurley, chief nursing officer at SDNAMC, performed an organizational assessment of physical sitter utilization and practices. She worked closely with the Falls Committee to ensure all appropriate tactics were deployed, held meetings with staff to discuss concerns around PCT reassignment and workload burdens placed on staff, met with families of patients in need of physical sitters, and interviewed physicians who commonly ordered physical sitters. She performed an initial review of the literature on falls prevention strategies, including an emerging solution known as virtual sitter technology (VST).
A New Technology
The VST strategy leverages existing technology, providing live-stream video of patient activity to a central monitoring station. Literature on VST was limited, se we contacted hospitals currently engaged in the strategy to gain experiential information as well. We evaluated VST solutions available in the market and chose the AvaSys system (AvaSure, Grand Rapids, Mich.) for its portability, audio functionality, and because it does not require integration with the nurse call system.
 |
| Figure 1. Virtual sitter technology installed on mobile cart and positioned at the foot of the patient’s bed. |
 |
|
| Figure 2. Remote observation station. |
AvaSys is a remote patient observation system that enables both visual and audio monitoring of patients at risk of self-harm, including falls, removal of lifesaving devices, and elopement. A mobile cart stationed in the patient room has a camera with pan and zoom capability and high-quality, two-way audio (Figure 1). It connects via Wi-Fi to a remote observation station manned by a PCT, who watches over as many as 10 patients simultaneously on a single screen (Figure 2). When a patient shows signs of getting out of bed, the monitor tech uses the audio to ask the patient to stay put while simultaneously alerting a nurse via phone or radio. If the sitter is unable to redirect the patient, a STAT alarm on the unit sounds.
Remote monitoring has enabled SDNAMC to expand the population of patients being monitored. Our evidence-based fall-risk assessment tool, which is filled out within our electronic health record upon admission, uses a set of parameters that captures a large percentage of the patient population and yet still misses patients who wind up falling. It focuses on several factors, including history of falling, age, level of confusion, vertigo, gender (men fall more), medication use, problems with toileting capability, and performance assessment on a specific task (such as rising from a seated position). Upon initial and ongoing patient contact by hospital staff, a total risk score for the patient is determined.
Despite our best attempts at identifying patients at risk for falls, it isn’t always the 86-year-old with a urinary tract infection who falls; it’s often a 36-year-old man who has had a gallbladder removed, wakes up in the middle of the night to venture toward the bathroom for the first time in a couple days, and won’t ask for assistance. So where our conventional assessment might have four patients needing a sitter, we have 10 cameras available, so using a modified risk assessment we are using VST with patients who demonstrate some memory loss but are not at high risk for falls, patients under the influence of drugs or alcohol; those who are not impulsive and have good cognition, but are on prone to fall injury because they are on anticoagulants or have osteoporosis; and those who are only temporarily at risk, coming from the ICU or post-surgery.
Staff Buy-In
Upon explaining the VST system to nurses, physicians, and PCTs, the feedback was uniformly positive. Nurses and PCTs often see sitting as a distraction from patient care, while staffing and managing sitters is an ongoing challenge. The staff’s enthusiasm for video monitoring served as a catalyst in the decision to move forward. Our chief medical officer was an early champion as well and served as a liaison to the medical staff, answering questions related to the new strategy.
The implementation process was very successful. The system was near “turn key” and required minimal resources to initiate. The manufacturer provided resources, including job descriptions and educational tools for the monitoring technicians, as well as policies and protocols, which we tweaked based on our organizational culture and needs. For example, our monitor techs go to the patient room to introduce themselves to the patients and family, explaining the system and their role in keeping them safe. The IT implementation was relatively smooth (installation of server software and wiring the monitor), and the on-site support was outstanding.
The system is deployed in a manner that meets regulatory demands and maintains maximal patient privacy. Although VST is capable of recording, that feature is turned off during regular observation. It has a privacy mode; nurses use audio to ask the monitor techs to turn off the video feed while a patient is being attended to. On the monitor screen, that room shows up as blank until the nurse signals it is time to remove privacy mode. An LED light in the room lets patients know whether privacy mode is on or off.
Results
Initial findings have demonstrated positive results. Figure 3 documents the monthly occurrence of patient falls for the locations where we have deployed VST. August demonstrates the lowest number of falls for 2014 year-to-date, with a 47% reduction in falls compared to July. We did note an increase in the overall number of falls in September but are still encouraged by the anecdotal observations and reports of prevented near-miss falls from our staff. It is important to note that zero falls with injury have occurred since implementation of our VST solution.
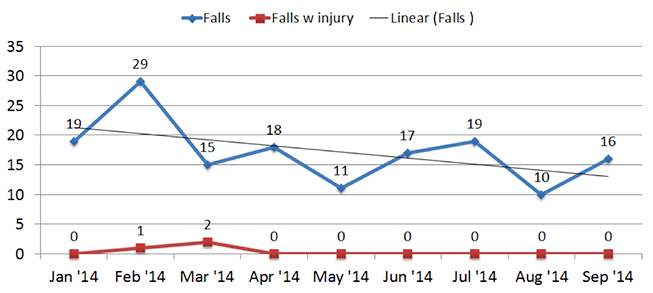 |
| Figure 3. Incidence of Falls at SDNAMC after Implementation of Virtual Sitter Technology |
Remote monitoring with VST has expanded SDNAMC’s capacity to monitor at-risk patients while achieving labor cost savings. In July, August and September of 2014 the remote monitors provided 5,922 of surveillance that previously would have involved one-on-one monitoring, saving $50,000 in labor expense. An additional 10,675 hours of surveillance occurred that was beyond what would have been possible with human sitters, using an expanded tier of risk assessment.
Experiential Accounts
Jack Holman, our first monitor tech, who now trains others on the new system, used to do one-on-one sitting with patients. “I must admit I had my doubts when I was going through the training. I thought, ‘How is the system going to prevent patients from falling, how can I do this when I’m not actually there with the patient?’ It has turned out well. I have now become really good at reading people’s body language. It takes about four hours to understand a new patient and what their next movement is going to be.”
In addition to preventing several falls, Holman has alerted staff to prevent patients from pulling out their IVs or other tubes. On one occasion, he alerted staff when he observed a patient who appeared to increase his respiratory rate, possibly preventing a more serious respiratory event.
Zenoba Peterson, an RN on a medical-surgical unit, said the system is instant in terms of starting monitoring of an at-risk patient, a far cry from previous practice. “You would get an order for a sitter at 3 p.m., but the actual sitter wouldn’t get to the room until the night shift. This is such a change to be able to have a monitor in the room and someone to alert me if the patient needs me.”
Bed alarms, Peterson notes, often sound only when the patient is swinging his or her legs out of bed, too late for a nurse to respond. “And a bed alarm can’t talk to the patient and tell him to please wait for the nurse,” she adds.
Family members of patients who need round-the-clock observation have been the biggest supporters of the video system. Patty McKay, whose husband David McKay had a stroke at age 74, said it was especially valuable for peace of mind. “When he first came to the unit, he was so restless he was very hard to control. The bed rails did nothing. So the monitor was brought in to watch him, and whenever he was trying to get out of bed the nurses would respond immediately. When I would go home at night it was very reassuring to know someone was watching over him.”
Conclusion
Early results of VST implementation for prevention of falls are positive, but more data is needed over a longer period of time to more accurately assess the impact of VST. A substantial increase of virtual sitter hours over historical physical sitter run rate brings into question whether these patient hours accurately represent patients who would have been assigned a physical sitter.
After further assessment, it was determined a second tier within the sitter criteria had been unofficially established through day-to-day decision making. Patients meeting criteria but not assigned a sitter often wound up being cared for by a charge nurse, assigned to a room nearby the nurses station or had family constantly present. This practice may prolong the forecasted return on investment in VST technology.
Additionally, significant increases of constant patient surveillance hours are well documented. This increase in surveillance will prevent falls from occurring while reducing labor costs associated with physical sitters. Not included in the original financial return projection was the prevention of falls with injury. As more data is collected, this should be accounted for as well.
Since the implementation of our initial strategy, other facilities within HCA have deployed the VST solution. We see this as a catalyst for increasing our learning and proficiency with this new strategy. Early discussion on expansion of units and centralization of the video monitoring station among facilities has begun.
Jane McCurley is chief nursing officer (CNO) of St. David’s North Austin (Texas) Medical Center. She has more than 30 years of experience in nursing and previously served as CNO of North Hills Hospital in North Richland Hills, Texas, where she advanced a wide range of quality initiatives. McCurley may be contacted at Jane.Mccurley@stdavids.com.
James Pittman is associate chief nursing officer for SDNAMC. He has served as director of the hospital’s Kidney Transplant Center and is vice chairman for the Organ Procurement and Transplantation Network and the United Network for Organ Sharing transplant administrators committee. Pittman may be contacted at James.Pittman@HCAHealthcare.com.
Mccurley, J., & Pittman, J. (2014). A new approach to fall prevention in inpatient care. Patient Safety & Quality Healthcare, 11(6), 50–53.
References
Boushon, B., Nielsen, G., Quigley, P., Rutherford, P., Taylor, J., Shannon, D., & Rita, S. (2012). How-to guide: Reducing patient injuries from falls. Cambridge, MA: Institute for Healthcare Improvement. http://www.ihi.org/resources/Pages/Tools/TCABHowToGuideReducingPatientInjuriesfromFalls.aspx
Centers for Medicare and Medicaid Services. (2008, April 14). CMS proposes additions to list of hospital-acquired conditions for fiscal year 2009. http://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-Sheets/2008-Fact-Sheets-Items/2008-04-14.html
Williams, T., Szekendi, M., & Thomas, S. (2014).An analysis of patient falls and fall prevention programs across academic medical centers. Journal of Nursing Care Quality, 29(1), 19-29. doi: 10.1097/NCQ.0b013e3182a0cd19.
