New York State Coalition Improves Communication for Care Transitions
By Fred Ratto Jr, BA; Sara Butterfield, RN, BSN, CPHQ, CCM; Christine Stegel, RN, MS, CPHQ; and Joseph O’Donnell, MA, MS
Contributing Authors
Special thanks to contributing authors Karen Houston, RN, MS (Albany Medical Center); Sandra Lawlor, RN, BSN (Evergreen Commons); Michelle Moore, RN, BSN (Barnwell Nursing & Rehabilitation Center); and Judy Vopelak (VNA Home Health) for providing their expertise and perspectives on the positive outcomes achieved by the Albany Care Transitions Coalition.
The effective transfer of patient care information is essential to a patient’s continuity of care whether conveyed in written documents, verbally, or electronically. Ineffective communication and transfer of patient information has been associated with medical errors, patient harm, and patient dissatisfaction. The Joint Commission Center for Transforming Healthcare estimates that “80 percent of serious medical errors involve miscommunication between caregivers when patients are transferred or handed-off” (2013). These errors and adverse events can result in hospital readmissions and poor continuity of care.
To improve patient care continuity, the Affordable Care Act (ACA) of 2010 encourages providers to shift their focus away from fragmented and episodic care to a more holistic approach that emphasizes improved communication across settings. Care coordination is supported through the Centers for Medicare and Medicaid Services’ (CMS) Community Based Care Transitions Programs (CCTP) whereby acute care providers partner with community-based organizations to reduce readmissions of Medicare beneficiaries. New payment models such as Accountable Care Organizations (ACOs) likewise have encouraged hospitals and providers to work together as networks, sharing information and resources to improve care and reduce cost, with financial incentives for savings and quality.
The ACA’s Hospital Readmissions Reduction Program, which penalizes hospitals for readmissions in less than 30 days for certain diagnosis, has compelled healthcare providers to improve communications in order to reduce their readmission numbers. Since August 2008, CMS has directed Medicare-funded Quality Improvement Organizations (QIOs) to build community coalitions and perform root-cause analysis on the drivers of poor transitions of care and avoidable readmissions in order to improve communication and care coordination across the healthcare continuum.
Environmental Scan of the Community
The healthcare delivery system within the capital region of New York state has embraced rapid cycle change and partnership building in order to improve care coordination. In 2011, Albany Medical Center (AMC), a 734-bed facility with the busiest trauma center in the state, wrestled with the same issues as most acute care facilities: the need to decrease length of stay and maintain the quality of care delivery while treating patients with increasing needs. AMC’s director of continuum of care, Karen Houston, RN, MS, was asked to oversee that institution’s readmissions reduction program, which emphasized specialized education of case managers and discharge nurses about readmissions and high-risk patients.
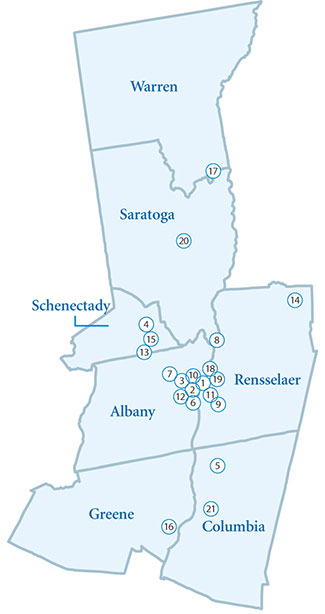
In collaboration with AMC, the Care Transitions Project Team from IPRO, the Medicare Quality Improvement Organization for New York state, facilitated development of an innovative community coalition partnership, which included the hospital, several skilled nursing facilities (SNFs), a home health agency (HHA), and hospice provider covering a seven-county region that includes Albany, the state capital (Figure 1). The coalition focused on improving communication and care coordination while managing clinically complex, high-risk patients across the healthcare continuum. IPRO assisted the coalition with a community-based root-cause analysis incorporating data drill down and tracking to analyze the drivers of readmissions within the community. The program was enhanced with coaching programs that used hospital discharge nurses to call high-risk patients is discuss appointments, medication adherence, and follow-up physician care.
 |
|
| Figure 1. Coalition Geographic Definition The numbers indicate how many coalition providers are in each county. |
A specialized discharge program for high-risk patient populations was established by Dr. Kevin Costello, an AMC hospitalist with expertise in gerontology. High-risk patients were discharged into the community with safety-net support from Dr. Costello and VNA Home Health, a Medicare-certified home health provider, prior to the patient’s first post-discharge primary care visit. AMC also partnered with VNA Home Health to focus on patients who transitioned to sub-acute care programs in SNFs, with a transition nurse carrying out specialized care planning in collaboration with the sub-acute care management team.
Even with these interventions, AMC and the community of surrounding providers still saw opportunities to reduce readmission rates and gaps in communication between settings. All-cause 30-day readmission numbers approached 21% in 2011 for AMC, higher than New York’s statewide average of 20%. In addition, the healthcare environment in the capital region of Albany was in flux as health systems merged and providers aligned services. A shift in healthcare policies through the ACA compelled providers who were once competitors to look at each other as partners-in-care as quality became more significant than quantity and hospitals were penalized for unnecessary readmissions. AMC recognized that healthcare providers outside their four walls had to be engaged for improvement to take place.
Albany Care Transitions Coalition
Collaboration began in earnest in early 2012. According to Houston,
The goal was safe, effective transitions to the next level of care. Many of the skilled nursing facilities in the area approached AMC to say that we really need to all look at improving some gaps in communication and coordination from discharge through transition to the next level of care. Our group began to meet monthly, the membership grew, and it was very, very exciting.
Houston says that many of the independent skilled nursing facilities recognized AMC as a large referral source, with AMC discharging more than 1,000 post-acute patients to SNFs per year.
Surrounding facilities in the region wanted to improve relations and communications in order to improve quality and patient outcomes. They recognized that readmissions and care coordination involved them as well, and as Michelle Moore, RN, BSN, director of nursing at Barnwell Nursing and Rehabilitation stated, “Long-term care has become more acute. Getting the SNF staff more comfortable with providing that care is important. Partnering with acute care is important. If AMC is successful, then we are successful.” IPRO also approached AMC to offer quality improvement tools, strategies, technical assistance, and data. “When we were approached by the facilities and IPRO, the timing was right, and our common goals aligned,” Houston stated.
In early 2012, AMC partnered with 28 SNFs, a home health care agency, and IPRO to establish the Albany Care Transitions Coalition (ACTC). Monthly meetings were used to address issues of poor communication and information flow among care settings. A root-cause analysis revealed an opportunity for improvement in communication between healthcare settings to decrease existing barriers to smooth transitional care management.
Communication Gaps
The lack of a standardized transfer-of-information document was identified as an opportunity for improvement. SNFs working with AMC were using different forms, the information transferred was not always consistent, and forms faxed between settings did not always make it to the right nursing unit. Person-to-person, cross-setting communication among clinicians was lacking. AMC and SNF providers did not have a standardized cross-setting contact list for clinical support regarding issues such as medication management and discharge planning. Information about the clinical capabilities of the individual SNFs was not always available for clinicians in the emergency department (ED). These issues, identified by the ACTC through the root-cause analysis, provided opportunities for improvement. The ACTC partners met monthly to share information and data, review case histories, and work as a team to implement solutions.
Transfer-of-Information Form
Research has indicated that standardized communication tools can improve safety and increase the amount of essential information provided to the ED (Leonard, Graham & Bonacum, 2004; Bean et al., 2004). As care environments become more complex, standardized communication tools can help prevent human errors and improve communication. Prior to the formation of the ACTC, SNFs that transferred residents to AMC’s ED used transfer forms with different formats and information. AMC had not made clear what information its ED required for triage and care planning. In an effort to improve this process, IPRO provided guidance and evidence-based communication tools to coalition partners. One of those tools, the Information to Reduce Acute Care Transfers (INTERACT) Nursing Home to Hospital Transfer Form, was adopted by AMC and the coalition SNFs, which resulted in improved transfer of information to the ED.
Cross-Setting Clinician Reporting
According to Dr. Eric Coleman (2003), coordination of care between settings often fails to safeguard that the necessary elements of the patient’s care plan developed in one care setting are communicated thoroughly to the care team in the next healthcare setting. For a successful transition to take place, clinicians need to be accountable for sending and receiving information, whether transmitted electronically, by fax, or verbally (Joint Commission, 2013).
In order to ensure more effective communication and avoid gaps in health information between settings, AMC and the ACTC incorporated a nurse-to-nurse reporting system in their discharge process. This process entails verbal communication between the hospital discharge nurse and the receiving SNF nurse regarding the patient’s discharge plan of care. Transitioning patients’ discharge summaries and instructions are reviewed as well as medication lists and patient assessment information. Critical patient information is sent via fax to the SNF nurse prior to discharge so questions about the care plan can be asked and further instructions or clarifications can be requested, such as details about tests, labs, and medications. Providers have indicated that this process has resulted in more effective care transitions between settings with fewer errors. Sandy Lawlor, RN, BSN, director of clinical systems at Evergreen Commons, observed, “There is a sense of comfort and recourse as the communicating nurses have a common understanding of the patient’s clinical needs they are transitioning, and they speak the same language.”
Electronic Health Records
Studies show that information technologies, including electronic health records (EHRs), have the potential to improve safety by assisting with decision making at the point of care (Gans et al., 2005). One strategy that the ACTC implemented successfully was to expand its EHR capacities to its network of coalition SNF partners by training, credentialing, and certifying SNF physicians and nurses to have access to AMC’s EHR system for their specific patient populations. This has facilitated greater access to health records for appropriate transitions and care planning. Previously this information was available only through paper access, which yielded less than half the health data of EHRs. This access to critical patient information provided another platform to prepare for the transition and care of patients.
Nursing Facility Capabilities List
Herndon et al. (2013) identify “lack of key information…and experience of hospital staff with SNFs, and thus an inaccurate perception of the assets and limitations of a particular SNF” as contributing to failure in treatment plans. Investigation of the initial baseline performance by ACTC members determined that AMC hospitalists and ED personnel required more information regarding which SNFs provide enhanced capabilities, such as IV antibiotics, PICC insertions, and TPN. IPRO assisted by providing the INTERACT Nursing Home Capabilities List, which each of the SNFs had completed. IPRO then aggregated the information into one main reference document. AMC has attached this document to its electronic systems platform for easier clinician/hospitalist access within the ED for purposes of developing care plans.
Emergency Department 24/7 Access Center
Patients transitioning from the community to the ED are at high risk for complications due to incomplete or missing information. Efforts to improve communications between community clinicians and the ED can improve coordination, assist with reducing unnecessary transfers, and improve the quality of patient care (Pearson & Coburn, 2013).
To streamline patient information transfers when SNF residents are transferred to its ED, AMC developed the Access Center, composed of AMC support staff coordinators who assist with incoming transfers to the ED. They support facilities and other healthcare providers with incoming patient transfers by receiving necessary health information such as diagnosis and special care needs or requirements such as specialists and treatments upon transfer. This platform also supports physician-to-physician information sharing across settings. SNF physicians sending residents to the ED for evaluation can communicate their assessment of patient status and expected plan of care at the time of transfer. AMC Access Center staff collaborated in coalition meetings to explain Access Center capabilities and uses. ACTC partners have reported positive outcomes and improved communications using the AMC Access Center as a tool for improved transitions.
Home Health Transitions Program
VNA Home Health, an ACTC partner, collaborated with AMC to develop and implement a sub-acute transitional care program. AMC social workers and clinicians communicate closely with VNA Home Health hospital liaisons who refer patients who may require home care services after an acute rehab stay in a SNF. A home-health transition nurse visits referred patients in the hospital to perform initial assessments. These patients are followed by the transition nurse into sub-acute facilities where further collaboration and communication takes place with nursing staff, patients, and their families about therapeutic planning needs. The transition nurse uses this information to develop a care plan that streamlines the patient’s transition back to the community.
This program has been successful, with an increase in referrals and a significant drop in rehospitalizations. Judy Vopelak, community liaison manager for VNA Home Health, notes:
We deal with the same issues in all settings and face similar challenges. Coalition members all have the same goal for improved care transitions through enhanced communication. Participation with our partners in care has become a discovery process in finding commonalties for solutions.
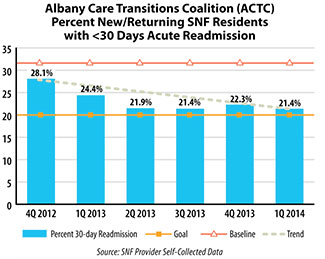
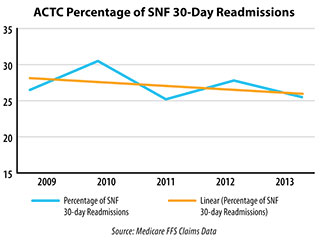
ACTC Intervention Results: Better Transitional Care, Improved Relationships, and an Award
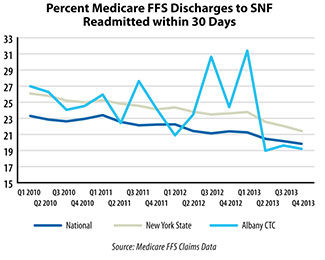
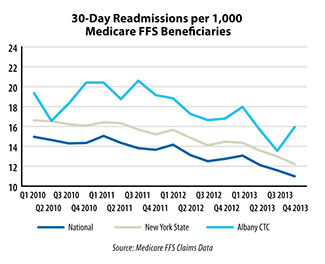
The bundle of ACTC interventions resulted rapidly in positive outcomes. All-cause, 30-day readmission rates among coalition SNF providers decreased from 28.1% in Q4 of 2012 to 21.4% in Q1 of 2014 (Figure 2). Houston commented that this success has been significant and that some coalition SNF members have reported zero readmissions in their monthly reports. This trend is particularly significant since the percentages of discharges to the SNF setting has increased by almost 6% (Figure 3), while all-cause 30-day SNF readmission rates have continued to decrease (Figure 4), well below New York and national averages (Figure 5). The ACTC SNFs utilize the INTERACT Quality Improvement Tool for Review of Acute Care Transfers to screen for potentially avoidable readmissions, which are reviewed with Houston on a monthly basis.
 |
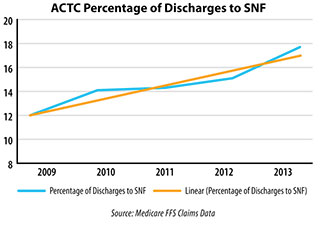 |
| Figure 2. Skilled Nursing Facility 30-Day Readmission Trends | Figure 3. Skilled Nursing Facility Discharge Trend |
 |
 |
| Figure 4. Skilled Nursing Facility Readmission Trend | Figure 5. Skilled Nursing Facility Readmission Comparison |
AMC’s 30-day all-cause Medicare fee-for-service (FFS) readmission rates dropped as well. In 2012, coalition members established a goal to reduce those readmissions by 5%, which was exceeded following the coalition’s interventions. For one target measure, the data demonstrated a relative improvement of 35% in Medicare FFS 30-day all-cause readmission rates from 21% in June 2011 to 13.8% in December 2013 (Figure 6).
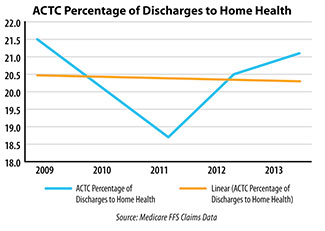
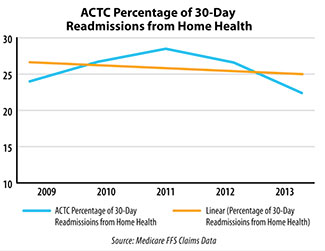
Home healthcare also benefited from the bundled interventions. Thirty-day readmissions dropped from 21.5% in Q1 of 2009 to 20.9% in Q4 of 2013 for patents discharged to home health from AMC. This positive trend is significant since the percentages of discharges to the home-health setting has increased (Figure 7), while 30-day all-cause SNF readmission rates have continued to decrease (Figure 8).
The sub-acute home health project through VNA Home Health yielded greater results, with a 3% all-cause readmission rate reported for 2013 for patients transitioning from short-term rehabilitation facilities to home with home care in place (Figure 9).
 |
 |
| Figure 6. Albany Coalition 30-Day All Cause Medicare FFS Readmission Comparison | Figure 7. Home Health Discharge Trend |
 |
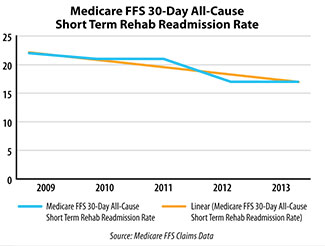 |
| Figure 8. Home Health Readmission Trend | Figure 9. Short-Term Rehab with Home Health Intervention Readmission Trend |
In addition to the improvement in readmission numbers, patient satisfaction surveys conducted by Houston with patients and families transitioned to short-term rehabilitation facilities following an acute hospital stay have revealed continued improvement. From March 2013 to the first quarter of 2014, an improvement rate of 29% was shown in patient satisfaction when queried as to whether their therapy needs were met (71% to 100% very satisfied in 2014).
“Improving gaps in communication” for care coordination was the major motivation for the ACTC members to join the project in early 2012, and much has been achieved. In June 2014, the ACTC Coalition, led by Houston, received the IPRO Quality Award for Excellence in Care Transitions for achieving a 30% relative improvement in Medicare FFS beneficiaries’ 30-day all-cause readmissions.
Cross-setting communication has improved dramatically. Nurse-to-nurse reporting as part of the discharge process has improved the accuracy of patient care plans by hospitalists and acted as an impetus for improved medication reconciliation. The standardized transfer-of-information form and the nursing home capabilities list have streamlined the flow of vital information necessary for smoother transitions and patient care. Expansion of AMC’s EHR to SNF liaisons and their clinicians has dramatically improved access to patients’ health records and assisted with transitions, patient care, and safety. The partnership with an HHA that specializes in a sub-acute care transition program has reduced short-term rehabilitation patient readmissions and improved the quality of care.
The Coalition Environment: The Number One Intervention for Improving Communication
Houston explained, “The relationship building and the culture change that took place in the ACTC coalition itself was remarkable.”
AMC and the community providers reported that they were able to meet face-to-face and develop relationships for the first time. As teams from different care settings learned more about each other and the complexities of the patient populations they serve, they developed mutual respect. One clinician partner commented, “When we contact each other, we know who we are talking to. There is an established relationship already, and it makes it easier to communicate and navigate through solutions about a transition or issue.”
Houston elaborated that in this new environment there is now a willingness to say, “Where did we go wrong, and how can we fix it? There is no blame game. There is more of a sense of team among the cross-setting providers.”
In this new “coalition environment,” the ACTC has been able to develop cross-setting relationships and implement standardized tools and systems that improve the transfer of information between settings and coordination of care. In addition to improving relationships among care settings, coalition meetings also improve safety and quality (Pearson, 2013).
When asked if she was proud of the recent accomplishments of AMC and the coalition, Houston responded, “Yes, we are excited and proud. It is a team effort…there are a lot of opportunities. We have a great meeting every month, and we always have new ideas to implement.” And the coalition continues to grow, there are now more than 34 healthcare provider members over a seven-county region. Her advice to other hospitals regarding coalition work is, “Get involved. Go to the table and go often.”
All of the authors work for the Care Transitions Team at IPRO, New York State’s Medicare Quality Improvement Organization.
Fred Ratto is a quality improvement specialist for the Care Transitions Team and a graduate student at the School of Public Health in Albany, New York. Previously, he served at-risk populations with intensive case management through the Office of Mental Health Community-Based Programs and as a regional specialist for aging and disabled populations in the New York State Department of Health HCBS Waiver Programs.
Sara Butterfield is IPRO’s senior director of healthcare quality improvement and project lead for the Centers for Medicare & Medicaid Services’ (CMS) 11th Scope of Work Coordination of Care initiative. Since joining IPRO in July 1998, Ms. Butterfield has coordinated collaborative partnerships with acute care hospitals, home health, Hospice, skilled nursing facilities, and private physician practices on a cross-setting, multidisciplinary level to facilitate performance improvement initiatives in support of CMS’ project objectives. She may be contacted at Sara.Butterfield@area-I.hcqis.org.
Christine Stegel is a senior quality improvement specialist at IPRO. Stegel has more than 25 years of home healthcare experience, including direct care delivery, multidisciplinary supervision, performance improvement, and operations management.
Joseph O’Donnell is IPRO’s senior analyst for the Centers for the CMS 11th Scope of Work Coordination of Care initiative. While at IPRO, O’Donnell has developed statistical and mapping approaches to defining geographic service areas, designed and produced series of statistical reports for distribution to providers, assisted providers in the analysis of provider-collected data, and performed other analyses in response to requests from initiative team members.
This material was prepared by the Atlantic Quality Innovation Network (AQIN), the Medicare Quality Innovation Network-Quality Improvement Organization for New York State, South Carolina, and the District of Columbia, under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U.S. Department of Health and Human Services. The contents do not necessarily reflect CMS policy. 11SOW-AQINNY-TskC.3-15-03.
References
Agency for Healthcare Research and Quality (AHRQ). (2012). Hospital survey on patient safety culture. AHRQ User Comparative Database Report. Retrieved August 18, 2014, from http://www.ahrq.gov/professionals/quality-patient-safety/patientsafetyculture/hospital/2012/index.html
Bean, W. F., et al. (2004). A standardized transfer improves communication between extended care facilities and the emergency department. Annals of Emergency Medicine. 4, 44.
Coleman, E. (2003). Falling through the cracks: Challenges and opportunities for improving transitional care for persons with continuous complex needs. Journal of the American Geriatrics Society, 51, 549-555.
Gans, D., Kralewski, J., Hammons, J., & Dowd, B. (2005). Medical groups adoption of electronic health records and information systems. Health Affairs, 24(5), 1323-1333.
Herndon, L., Bones, C., Bradke, P., & Rutherford, P. (2013). How-to guide: Improving transitions from the hospital to skilled nursing facilities to reduce avoidable rehospitalizations. Cambridge, MA: Institute for Healthcare Improvement.
Joint Commission Center for Transforming Healthcare. 2013 facts about the hand-off communications project. Retrieved August 18, 2014, from http://www.centerfortransforminghealthcare.org/projects/detail.aspx?Project=1
Leonard, M., Graham, S., & Bonacum, D. (2004). The human factor: The critical importance of effective teamwork and communication in providing safe care. BMJ Quality & Safety, 13 (Suppl. 1), i85-i90.
Pearson, B., & Coburn, A. (2013). Emergency transfers of the elderly from nursing facilities to critical access hospitals: Opportunities for improving patient safety and quality. Flex Monitoring Team. Policy Brief 32. Retrieved August 11, 2014, from http://www.flexmonitoring.org/wp-content/uploads/2013/07/PolicyBrief32-Transfer-Protocols-with-Appendix.pdf
