Unintended Consequences of Smart Pumps: Lessons Learned from a Root Cause Analysis
By Joan D. Wynn, PhD, RN; Lou Reida, MSN, RN; David C. Herman, MD, MSMM
Safety experts, policy makers, and regulators cite technology solutions as key strategies to create a safer healthcare environment (Kohn, Corrigan & Donaldson, 2000; Wachter, 2012). Infusion pumps with built-in decision support logic for dosing limits and clinical advisories are one such solution currently employed by many hospitals. These “smart” infusion pumps are designed with drug-specific safety software to help detect and correct IV pump programming errors to reduce medication errors and potentially prevent patient injury (Elias & Moss, 2011; Harding, 2011; ISMP, 2007; Vanderveen, 2007).
A critical dependence on decision support in the pump may be an unintended consequence of this type of technology and can lead to a different set of safety events if appropriate safeguards are not established. These safeguards are especially important when the pump safety software is updated or changed. Changes involving dosing algorithms may not be transparent to the end users and may lead to adverse patient events when there is erosion or suspension of critical thinking due to alert fatigue from non-credible alarms and cultural tolerance of pump workarounds (ISMP, 2007).
This case report presents findings of a series of events that occurred in August 2011 at Vidant Health, a 10-hospital health system in the Southeast, after a scheduled dosing update to IV smart pumps impacted medication administration across the health system. Subsequent to the event, a root cause analysis was conducted at the system level to examine active errors and latent system weaknesses. Breakdowns in system design are described using the principles of Reliability Culture as presented by Healthcare Performance Improvement (HPI, 2009). Findings resulted in a new approach to implementation, maintenance, and ongoing support for new technology solutions used in patient care.
Initial Event
The health system’s academic medical center (AMC) implemented IV smart pump technology in 2004. Initial implementation and ongoing maintenance was managed through the personal oversight of trained individuals. Over time, ongoing pump management was placed on “autopilot” with loss of one trained and assigned individual to oversee continuous improvement of infusion best practice. With suboptimal maintenance of the IV pump drug library, nursing staff frequently overrode IV pump alerts, which increased the risk of medication errors and patient harm.
Because nursing and pharmacy expressed concerns regarding differences in IV pump drug library concentrations, drug concentrations in the electronic health record (EHR), and clinical unit practice, the pharmacy team began to work with nursing to match drug concentrations in the IV smart pump to drug concentrations in the EHR. In August 2011, concentration changes were made to the dose of five medications in the software programming for nursing and anesthesia, then transmitted wirelessly to IV pumps. Two months after the update, an ICU nurse programmed the pump to deliver fentanyl to a mechanically ventilated patient. Soon after the pump delivered the programmed dose of fentanyl, the ventilator alarmed. The patient’s blood pressure and heart rate dropped. The nurse scanned the environment and immediately identified that fentanyl was programmed in mcg/kg/hr in the IV pump instead of mcg/hr. Fentanyl was typically ordered, dosed, and programmed in mcg/hr in this patient care unit. The IV medication pump was immediately stopped. Side effects of the overdose resolved quickly without further patient harm.
It was determined that the nurse unknowingly selected the anesthesia dose instead of standard nursing dose for fentanyl. That meant a higher dose of medication was delivered to the patient than was intended. The nurse chose the wrong concentration because she thought there was only one concentration of fenatnyl available—mcg/hr—as had always been the case. The smart pump features an “anesthesia only” mode, which allows anesthesia to quickly access anesthesia-specific drugs, concentrations, and limits. When concentration changes were made to the five medications in software programming for nursing and anesthesia, the anesthesia-only option was unknowingly made available for nurses as well as anesthesia. As a result, the anesthesia drugs, concentrations, and limits were sorted to the top of the medication list and accessible by nursing.
Immediate Actions
The nurse immediately notified the charge nurse and patient care coordinator that the nurses’ view of the medication list had changed in the IV pump, and a patient had received a higher than intended dose of fentanyl. Within an hour, a team was assembled to investigate the issue. At that time, the team discovered anesthesia only concentrations appeared in the non-anesthesia, nursing drug profile. The executive on call communicated the situation to the chief quality officer. Communication went out to every hospital asking the house supervisor to conduct a check of all smart pumps to determine if the anesthesia drugs were appearing in nursing drug profiles for inpatients. In addition, a safety alert was posted to the health system’s intranet page and EHR log-in page. It was determined that the issue was occurring only at the academic medical center (AMC). Corrections to the drug library were made to suppress anesthesia drugs, concentrations, and limits from the nursing drug profile and wirelessly transmitted to all pumps across the AMC. This required that pumps be turned off and powered up and new patient be selected to activate the drug library changes. Biomedical, nursing, and pharmacy leaders rounded throughout the next 4 days to assure all pumps were located, powered off, and had accepted drug library changes. Twice daily check-in calls were scheduled to include the executive on call, nursing administrator on call, pharmacy, nursing, biomedical, information systems, and quality/safety leaders to assure resolution of risks.
The Root Cause Analysis
The analysis uncovered many gaps in smart pump management processes as well as cultural tolerance for smart pump workarounds. When concentration changes were made to the initial five medications, programmers in the pharmacy did not implement the additional step required to hide anesthesia doses from the nursing view. No standard operating procedure or checklist had been developed to assure this critical step was completed, and necessary information to bring awareness of the need for this step was difficult to locate in software instructional manuals. The infrequency of programming updates made it unlikely the programmer had sufficient experience to recall the process.
Once the updated drug profile was wirelessly transmitted to IV pumps, neither pharmacy nor nursing recognized the anesthesia dosage of the five drugs was at the top of the nursing IV drug profile. The pharmacy pump programmer had not been trained on the pump and assumed nursing had the same view as pharmacy in the editing software. There was no process for notifying nursing prior to medication profile updates or for verifying/visualizing the medication data set on a test IV pump prior to wireless transmission.
Upon initial implementation of smart pumps in 2004, there was a dedicated nurse project manager partnered with pharmacy for implementation and ongoing management. When the nurse project manager left the position in 2007, this person’s responsibilities were distributed, and ongoing pump management was not re-assigned to a nurse expert. In addition, pharmacy staff had made minor changes to drug profiles over the years and never experienced any issues, which contributed to the development of a false sense of security regarding the pump programming process. Furthermore, alerts were often overridden when fired due to the mismatch of drug concentrations in the pump and EHR orders, and this was the accepted cultural norm. Additional gaps were identified with nursing IV pump education, ongoing nursing competency, and a process for safety software compliance checks.
The root cause of the event was determined to be the absence of standard operating procedures for proactive pump management. Contributing causes included lack of an operational owner for ongoing pump management, and complacency post-implementation because no significant safety events had occurred.
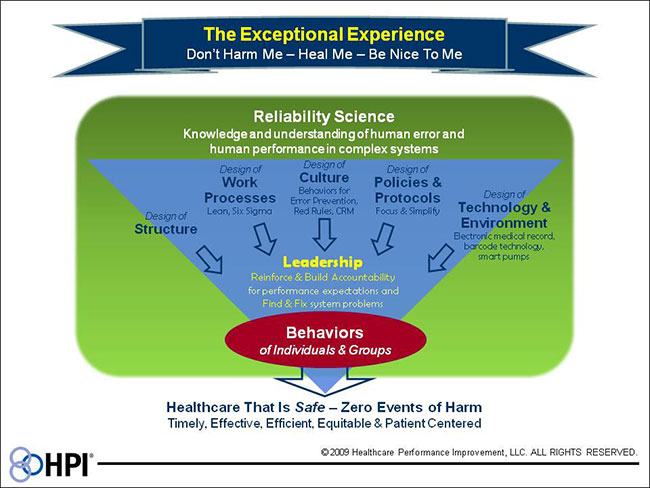
Figure 1. Reliability Culture Framework
Author note: Vidant Health adapted HPI’s reliability culture framework for internal use because patient and family engagement in quality and safety is a core organizational value. “Be Nice To Me” has been modified to “Partner With Me.”
Discussion
Healthcare organizations are adopting high reliability concepts from other complex industries such as nuclear power and aviation to improve patient safety and quality outcomes (Stockmeier & Clapper, 2011). One key concept that is important to understand in complex systems is the relationship between system design and the behavior of individuals. The reliability culture framework shown in Figure 1 (pg. 38) displays the relationship between system design and human performance in complex systems (HPI, 2009). The design of structure; work processes; culture; policies and protocols; and technology and environment influence and shape the behaviors of employees (Table 1, pg. 38). The behaviors and choices of employees drive outcomes in healthcare systems. The leader’s role is to facilitate and translate good system design into safe practices at the point of care. The employee’s role at the point of care is to make safe choices, utilize error prevention tools, and report unsafe system problems (HPI, 2009).
In the IV pump event, the system design and leadership role both contributed to the event (Figure 2). The impact of each of these areas is described below.
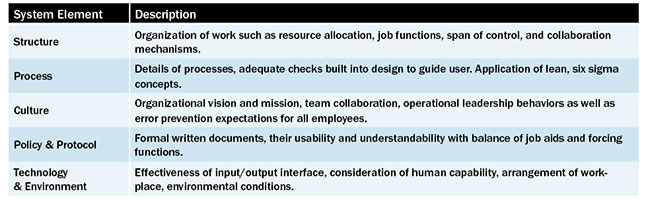
Table 1. Factors that Influence Employee Behaviors
Structure. Resource allocation was a system design flaw. The nurse project manager overseeing IV smart pump implementation was assigned to a different role, and the responsibility was not reassigned. Pharmacy lacked an RN partner to assist with medication updates to keep drug profiles current. Therefore, there was insufficient infrastructure to provide ongoing, proactive pump management.
Process. Key processes that were in place upon initial implementation were not documented and codified, resulting in process knowledge loss when initial staff left the program. These processes included notification and education of nursing during IV drug library updates and testing drug library update patient care pumps before hospital wide transmission.
Culture. Operational leaders did not dedicate adequate resources to address the emerging safety issues with IV pump management. There was a lack of a sense of urgency to correct the issues because there had been no serious events. That led to pharmacy and nursing believing that IV pump optimization was not an organizational priority, which contributed to the acceptable nursing norm of overriding alerts.
Policies and Protocol. The written policy and procedure for IV pump management was incomplete, and where processes and procedures did exist, they did not match actual practice.
Technology and Environment. The visual drug library display was different between nurse mode and pharmacy mode. The design of software without an obvious method to distinguish anesthesia mode from nursing mode was a contributing factor.
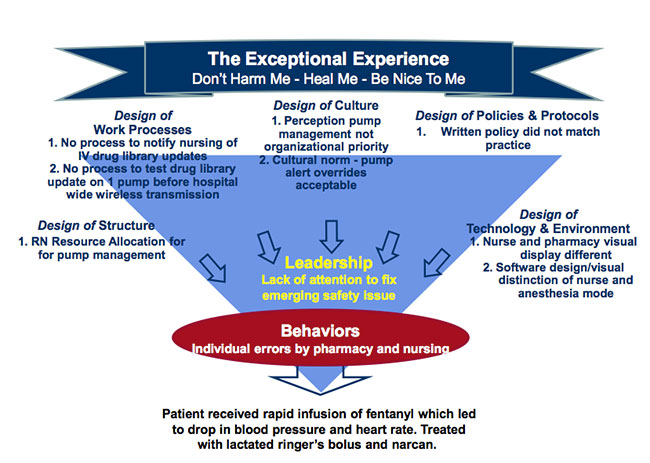
Figure 2. Event Analysis According to Reliability Culture Framework
Leadership Role. Staff expressed safety concerns regarding the fact that drug concentrations in the IV smart pumps did not match EHR drug concentrations. Requests were made for nursing assistance to “clean up” IV pump drug libraries. A nurse was assist to assist the pharmacy, but the work was extensive and more than the nurse could manage due to additional work responsibilities. Staff continued to express concerns up the chain of command, however leaders did not address them because they had competing priorities and did not appreciate the magnitude of the risk inherent with use of this technology.
The following actions were implemented based on root cause analysis findings:
- Radio frequency identification was implemented to locate IV pumps in a timely manner.
- A method was developed to assure the alignment of EHR medication concentrations, current available medication concentrations, and IV drug software.
- A GAP analysis was conducted with a best practice IV smart pump organization to determine opportunities to improve internal pump process management. An internal plan was developed for ongoing, proactive pump management that included policies and standard operating procedures for drug library change management, nursing education, and safety software compliance checks. The plan includes oversight of the process by a consistent interdisciplinary team, which includes a pharmacist and nursing informatics specialist—a new role for the organization.
- The vendor contract was closely reviewed with all applicable parties to assure necessary services to maximize patient safety.
Conclusion
Technology to support the work of people at the front line of patient care is a welcome solution to many safety issues and system weaknesses. If not implemented and maintained reliably, however, the technology can become a source of unintended complexity that can lead to safety events and patient harm. Ensuring patient safety cannot be delegated to a pump or to any piece of technology. Safe care requires human caregivers being mindful and making the right choices in order to safeguard patients. Organizations must carefully evaluate the manner in which they implement new technology and the systems they establish to perform updates and dissemination of enhancements.
The reliability culture framework provides a useful conceptual model in considering the interrelationships and system design. This model could be considered when conducting a failure modes effects analysis (FMEA) before institution of any new technology and used to develop persistent and defined operating practices that are more reliable and less dependent on individual actors than non-documented processes.
Joan Wynn is chief quality officer at Vidant Health and serves on the Board of the North Carolina Center for Hospital Quality and Patient Safety. Wynn earned a bachelor’s degree in nursing from the University of Maryland, a master’s in nursing from Johns Hopkins University, and a PhD in nursing from East Carolina University. She is also a certified professional in healthcare quality (CPHQ). Wynn may be contacted at JWynn@vidanthealth.com.
Lou Reida is the director of patient safety at Vidant Health. She earned a bachelor’s degree in nursing from the Univeristy of North Carolina at Chapel Hill and a master’s in nursing from East Carolina University. Reida is also a certified professional in healthcare quality (CPHQ) and a recent graduate from the AHA-NPSF Patient Safety Leadership Fellowship, Class 11.
David Herman is CEO of Vidant Health. He received his medical degree from Mayo Medical School and completed his residency in ophthalmology at the Mayo School of Graduate Medical Education. He received a master of science in medical management from the University of Texas-Dallas. Herman served on the Mayo Clinic staff from 1988 to 2011. He has served on the National Quality Forum (NQF) Outcomes Steering Committee and as Chair of the NQF Ophthalmology Technical Advisory Panel.
REFERENCES
Elias, B.L. & Moss, J.A. (2011). Smart pump technology: What we have learned. Computers, Informatics, Nursing, 29(3), 184-190.
Harding, A.D. (2011). Use of Intravenous Smart Pumps for Patient Safety. Journal of Emergency Nursing; 37(1), 71-72.
Healthcare Performance Improvement. (2011). The HPI SEC & SSER Patient Safety Measurement System for Healthcare. Appendix C-2.
Healthcare Performance Improvement. (2009). Reliability Culture.
Institute for Safe Medication Practices. (2007). Smart pumps are not smart on their own. Medication Safety Alert. Retrieved from http://www.ismp.org/newsletters/acutecare/articles/20070419.asp.
Kohn, L. T., Corrigan, J., & Donaldson, M. S. (2000). To err is human: Building a safer health system. Washington, D.C: National Academy Press.
Stockmeier, C. & Clapper, C. (2011). Daily check-in for safety: From best practice to common practice. Patient Safety & Quality Healthcare. 8(5), 30-36.
Vanderveen, T. (2007) Smart pumps: Advanced capabilities and continuous quality improvement. Patient Safety & Quality Healthcare, 4(1), 40–48. Retrieved from http://psqh.com/janfeb07/smartpumps.html.
Wachter, R.M. (2012). Understanding Patient Safety. New York: McGraw Hill.