Policies for the Use of Personal Mobile Devices in Surgical Suites
By Anne V. Irving, MA, FACHE, CPHRM, DFASHRM
Human factors studies indicate that distractions and multitasking increase the likelihood of error (Feil, 2013; Wiegmann, ElBardissi, Dearani, Daly, & Sundt, 2007). Allowing personnel to bring their cell phones, smartphones, or other mobile devices into a surgical suite introduces a new distraction into an already complex, noisy, high-stakes environment. Rather than assume that perioperative personnel will always use their best judgment, health systems should adopt formal, written policies, procedures, or guidelines for the use of personal devices in order to provide:
- Clarity regarding specific performance expectations
- A basis for enforcement, if instances of noncompliance are reported
- A clear message that patient safety is the highest priority at all times
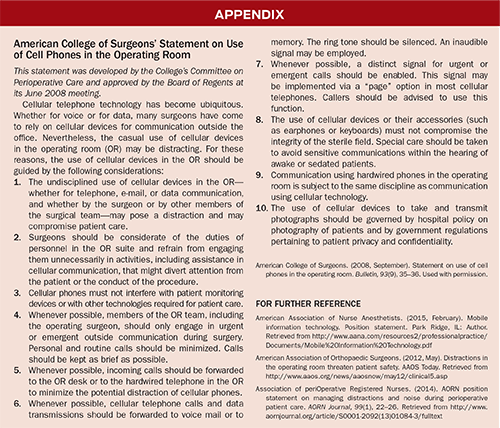
Several perioperative professional associations have weighed in on the use of personal mobile devices, including the Association of periOperative Registered Nurses, the American Association of Orthopaedic Surgeons, and the American Association of Nurse Anesthetists. See the appendix for the American College of Surgeons’ statement on the use of cell phones in the operating room and links to policies of other organizations.
Choosing a risk mitigation strategy
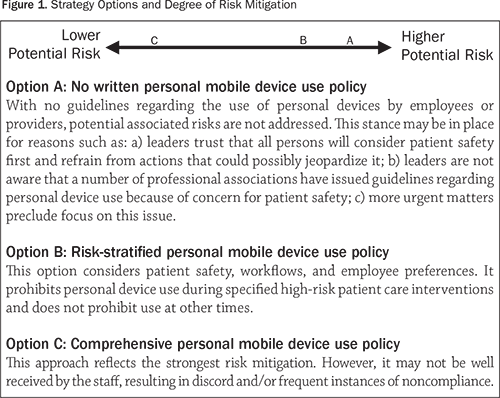
Healthcare leaders who decide to limit use of personal mobile devices during work hours must balance multiple considerations: patient safety, the impact on workflows in the organization, and the potential effect on employees and affiliated providers. Policies to control the use of personal devices can be perceived as positioned at various points on the risk mitigation continuum (Figure 1).
Option A
Choosing not to develop a formal policy regarding the use of personal devices (Option A) offers little, if any, risk mitigation. With no guidelines to follow, some staff members may feel compelled to look at or use their mobile device when engaged in direct patient care that requires their full attention. Such mental distractions increase the likelihood of medical errors.
Option B
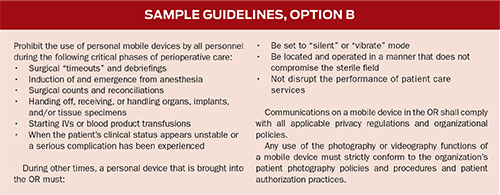
An alternative, risk-stratified policy (Option B) might include provisions such as prohibiting all personnel from bringing their personal devices into an OR suite for high-risk cases that meet one or more of the following criteria (which warrant specification and approval by the surgery/anesthesia leaders), such as:
- All “emergency” (non-elective) cases
- All cases with an American Society of Anesthesiologists classification of IV or higher
- Organ transplant cases
- Interventional radiology and cardiac procedures (diagnostic and therapeutic)
- Cases that require the services of a perfusionist
- Cases that are likely to require more than a specified number of hours to complete
- Cases in which the transfusion of blood products is anticipated or becomes necessary
Cases that do not meet one or more of the criteria for high risk should still be subject to guidelines, such as laid out in the following sidebar.
Option C
The strongest risk mitigation stance (Option C) is to implement a formalized, written policy that prohibits all perioperative personnel (providers with surgical or anesthesia privileges, nurses, techs, and independent contractors) from bringing their personal mobile devices into the OR suite or any other rooms where invasive procedures are performed. That means they must store their devices in a locker or wherever they keep their other belongings.
If someone urgently needs to reach a member of a perioperative team in the OR, he or she will call the main OR desk and request that the call be put through to the room where the intended recipient is located. The circulator—who is not scrubbed—typically answers telephone calls in the OR and will convey the information or question to the intended recipient.
Establishing this as the organization’s formal policy levels the playing field by not allowing selected providers access to their devices while denying others access. However, the policy will be effective only if medical staff and hospital leaders are willing to address reported instances of noncompliance without considering the offender’s hierarchical status. This policy should state that those who do not comply will be subject to disciplinary action in accordance with the applicable organizational medical staff peer review and human resources policies, whichever apply.
Prohibiting personal mobile devices in this environment mitigates risk by:
- Removing a potential source of cognitive distraction, thereby reducing the potential for errors of omission or commission
- Sending an unequivocal message that leaders expect all persons in the OR to give their full attention to the patient and their assigned perioperative responsibilities
- Eliminating the organization’s potential legal exposure (and encumbrances to the defense of otherwise defensible claims) if a perioperative claim arises and the plaintiff counsel learns through discovery that one or more of the perioperative staff had their devices in the OR and made use of them at some point during the case
Special exceptions should be clearly described in the policy. One exception to consider involves the anesthesia provider. It is not uncommon for the on-duty team of anesthesiologists to designate one individual as the “lead” for the day; the person serving in that role may need a phone or device to stay in communication with others in order to manage case assignments or adjustments.
Other considerations
All policies should indicate which departments or areas in the organization they apply to. In addition to the surgical suites (inpatient and outpatient), policies regarding the use of personal devices should apply to any area where invasive procedures are performed, including the cardiac cath lab, the electrophysiology lab, the interventional radiology suite, the diagnostic imaging department, the labor and delivery surgical suite, the emergency department, and the patient’s bedside (when resuscitation interventions or invasive procedures are underway).
Health system leaders may prefer to develop a policy on this subject that applies to all hospital departments and units or any other patient care delivery venue, specifying what is prohibited or permissible in each, rather than issuing a policy that applies solely to the perioperative areas.
Summary
When multiple professional associations issue practice guidelines on a topic identified as pertaining to patient safety, health system leaders should take notice. It is time to issue a formal policy on the staff’s use of personal devices, particularly when working in a clinical procedural area.
Choosing to defer attention to this matter could result in patient harm. From a risk management perspective, harm resulting from the use of personal devices such as cellphones and smartphones would appear to be very difficult—if not impossible—to defend. Advocates of patient safety are encouraged to take action in this area sooner rather than later.
Anne Irving is assistant vice president, risk management, for Premier Insurance Management Services. She provides a wide range of risk management educational and consultative services to health system members of the American Excess Insurance Exchange, RRG. She may be contacted at Anne_Irving@Premierinc.com.
The information provided herein by Premier Insurance Management Services is intended for illustrative purposes only. Recipients must obtain input from administrative, medical staff, and nursing leaders as well as legal counsel in the development, revision, and implementation of this type of policy, procedure, or guideline.
References
Feil, M. (2013). Distractions and their impact on patient safety. Pennsylvania Patient Safety Advisory, 10(1), 1–10. Retrieved from http://patientsafetyauthority.org/ADVISORIES/AdvisoryLibrary/2013/Mar;10(1)/Pages/01.aspx
Wiegmann, D. A., ElBardissi, A. W., Dearani, J. A., Daly, R. C., & Sundt, T. M. (2007). Disruptions in surgical flow and their relationship to surgical errors: An exploratory investigation. Surgery, 142(5), 658–665.
