Interoperability in the Perioperative Suite: Promise and Reality
By Charlie Berg, BA, BSEE
In recent years, hospitals have made great strides in the adoption of electronic health records (EHR). As of 2014, 76% of hospitals in the United States were employing an EHR system to manage clinical information (American Hospital Association, 2015). The perioperative staff is now looking for improvements to their workflow and work environment from these electronic systems, seeking patient-safety focused integration of information carefully selected from the growing flood of electronic data. This article will explore the perioperative environment and look at some of the challenges to integrating with electronic systems and devices, extracting data that is relevant to clinical staff, and providing access to crucial data at each perioperative phase.
The perioperative environment
Patient care in the perioperative suite requires highly collaborative teamwork. During the perioperative process, clinicians from several disciplines need to attend to the patient in a simultaneous, real-time fashion. A single patient will be treated by multiple nurses, surgeons, anesthesiologists and anesthetists, radiology technicians, lab technicians, and blood bank staff. Additional support staff—sterile supply staff, environmental and infection control staff—can also impact patient safety outcomes. Highly technical equipment, instruments, medications, blood products, and supplies must be planned and prepared to be delivered at just the right time, frequently sourced from different departments (e.g., central supply, sterile instrument processing, patient transport, pharmacy, blood bank, surgical pathology). Additionally, OR staff must integrate their work with other hospital departments, such as recovery units, surgical clinics, radiology, laboratory, emergency department, critical care units, and others. For any given team, the mix of clinical and support staff can change from day to day, making it difficult for any single team to repeat a single surgical process the same way each time.
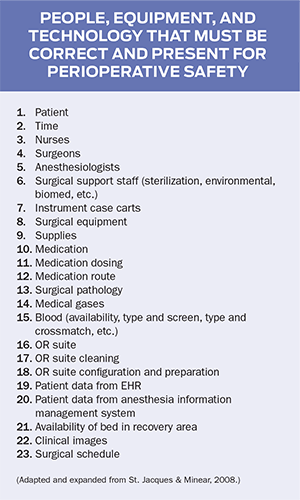
Other than a quick determination of the facts pertaining to a particular procedure, perioperative clinicians and associated staff have little time or opportunity to become familiar with individual cases. This lack of knowledge about patients could predispose perioperative team members to errors such as patient misidentification, miscommunication of the planned procedure, and omission of allergies or prophylactic antibiotics. Errors can be compounded by miscommunication between the primary surgical clinicians and the support staff who need to deliver the right resources at the right time. The sidebar on the facing page offers a short list of the various people, equipment, and technologies that must be present at the correct time for perioperative case safety.
Clearly, communication, scheduling, and monitoring are all key interactions required to manage the collaboration between clinical team members and support staff. Additionally, methods of acquiring, tracking, and notifying delivery of key assets play a significant role in managing the perioperative process. Various studies have demonstrated the efficacy of EHRs and Anesthesia Information Management Systems, also known as Anesthesia Record Keepers (ARK), in helping with communication (Dixon & Zafar, 2009; Lonergan & Ehrenfeld, 2012) and delivery of key assets (Ku, Wang, Su, Liu, & Hwang, 2011). However, as far as we have come in employing technology to improve perioperative workflow and asset management, we still have a ways to go.
EHR in the perioperative environment
With the numerous medical devices, ARK systems, robots, and other biomedical and IT-enabled devices in the perioperative suite, the risk of “information overload” is ever present. Although the EHR held promise as an integrator and presenter of key information during the perioperative process, it does not now, in itself, have the capacity to integrate with and visualize the vast array of devices and databases required by this environment. Current EHR technology does not meet the requirements of perioperative clinicians, administrators, or clerical staff. Surgical information systems as presently designed cannot keep pace with the demands of the perioperative process, providing only basic functionality in the areas of patient/case scheduling, case planning and management, staffing, OR suite management, and nursing perioperative documentation.
Integrating information in this environment requires bringing together many elements among the large set of technologies used in the OR and throughout the perioperative process. Workflow for clinicians must be made faster and easier, not slower and more complicated. This must be enabled by high levels of surgical equipment and software application interoperability throughout the perioperative process. Data interoperability would dramatically reduce data redundancy and errors. All pertinent data generated by clinical equipment should flow into clinical databases without manual reentry, thus increasing clinical acceptance and accuracy of data by reducing user workload and transcription errors. The EHR, as the central repository for much of the clinical information required in perioperative care, should support the capabilities required to achieve such interoperability. As noted by Dr. Neal Cohen in his article on coordinating perioperative care:
The electronic health record (EHR) is a tool to help document patient status and clinical needs, but in most cases the EHR is not the most effective way of communicating critically important information. In many respects, it provides too much information, making it difficult to identify the key issues; in other respects, access to all of the information may be difficult due to how the data are archived. (Cohen, 2015)
Additionally, a survey of 5,000 anesthesiologists revealed that the reason they did not use ARK systems was the perceived difficulty of integrating ARKs with existing EHRs (Trentman, Mueller, Ruskin, Noble, & Doyle, 2011). Better integration of the various IT components in the perioperative environment, therefore, is clearly a requirement.
EHRs and interoperability
Data exchange exists at two levels: the data encoding layer and the semantic meaning layer. Semantic interoperability ensures that two independent systems can share the same level of understanding of the communicated data. The form of information exchange is specific to a domain (e.g., perioperative, ED) and a context (e.g., clinical, pharmacy, laboratory). Semantic interoperability guarantees that healthcare professionals have a common understanding of the meaning of the transmitted data, beyond the machine-represented format.
Semantic interoperability is not possible without a defined terminology and ontology.* Language standards carefully define the set of items that can be defined, the attributes of the items, and the range of values these items take. Existing medical vocabularies (including SNOMED, and PNDS for perioperative documentation (Lundberg et al., 2012)) can partially assume this role; they are, however, incomplete and lack consistency for the perioperative environment (Ahmadian, 2011; Ahmadian, Cornet, van Klei, & deKeizer, 2011). Given the still-incomplete mapping of perioperative ontologies to these medical vocabularies, vocabulary adoption by EHR vendors is still in its early stages.
The data encoding layer defines the structure or format of data exchange (i.e., the message format standards) where there is uniform movement of healthcare data from one system to another such that the clinical or operational purpose and meaning of the data is preserved and unaltered. It ensures that data exchanges between IT systems can be interpreted at the data field level, representing the same values, units, metadata, and data provenance.
The current standard for interoperability between technologies in the perioperative environment (as in other clinical environments) is Health Level-7 (HL7 v2, v3) and its successor, Fast Healthcare Interoperability Resources (FHIR®©). HL7 v3 features the use of a Reference Information Model (RIM) as a common source for information content of specifications. The RIM is a high-level generic information model that represents all of healthcare. It is an essential part of HL7 v3 as it provides a precise representation of the semantic and lexical connections that exist between the information carried in the fields of HL7 messages. The standards mechanism for communicating the semantic information within the RIM is the Clinical Document Architecture (CDA). The CDA standards have been developed to include various data elements required for perioperative interoperability, but the current standard is still in trial implementation, and as such has not been fully implemented by all commercial EHR vendors (IHE Technical Committee, 2014).
In spite of the definitional limitations described above, most software systems and devices support at least some ability to provide HL7-based output of information from the EHR. However, EHR vendors often limit the information that can be input into their data repositories. Given that they work in a very competitive marketplace, EHR companies are also reluctant to communicate one-on-one to enable interoperability. Reports and HL7 interfaces are therefore limited in both the input and output of information to and from third-party data sources.
Furthermore, reports and HL7 interfaces are typically siloed by the particular module (e.g., perioperative, CPOE, pharmacological, etc.) within the EHR that they service. Some of this fragmentation is a function of how the clinical vocabularies and semantic communication standards have been organized and implemented by the EHRs. As a result, when information is needed that is resident in a specific software module unrelated to the perioperative process, those external sources of data may not necessarily contain the necessary common identifiers, making combination of information from those sources difficult or impossible.
Given the immaturity of some of the clinical vocabularies for perioperative communication across the many technologies in the surgical suite, and the similar immaturity of communication standards and mechanisms, it is no surprise that the EHR vendors lag behind on the effective implementation of interoperability capabilities. Future EHR advancement in interoperability can have a positive impact on the perioperative environment.
Interoperability in the perioperative suite
A vast array of technical data is continuously generated within the perioperative environment. In addition to physiological monitors, information is being captured by the ARK systems, the EHR, and even various medical devices, such as IV infusion pumps, medication dispensing units, and tagged supplies that utilize radio-frequency identification technology. This data is constantly being retrieved, documented, analyzed, and communicated to others, all within the daily routine of nursing care. The ability to retrieve and synchronize data is essential for clinical documentation and real-time problem solving, both for individual patients and the ICU as a whole. The capability to systematically and logically link ARK data, EHR information, and physiological monitors and other selected data sets into a cohesive workflow holds tremendous promise for improving care quality, patient safety, and clinical outcomes in the perioperative suite. However, as noted, the tools to provide such data fusion are in their infancy.
Data fusion by itself is not enough; it is critical that the information displayed is relevant to the clinical staff in the context of the care workflow in process. A central focus of most medical centers today is how to take one of the most expensive assets, the perioperative suite, and make it more efficient while improving the quality and outcomes of patient care. As already noted, verbal communication across changing care teams is often strained and imperfect. In addition, it often falls to a single person to inform the team of the pertinent clinical information required as part of the surgical process. The combination of a dependency on verbal communication, individual control of information, and fragmentation of data can create process breakdowns, leading to inconsistent care delivery or—worse—medical errors during care.
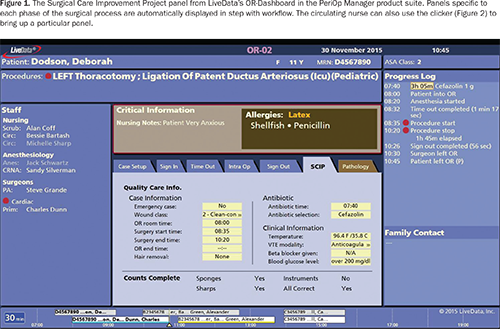
One way to leverage interoperability to improve team coordination and sustained process improvement is to utilize data across systems to create visual as well as verbal communication for clinical teams. One example of high interoperability in the perioperative suite is LiveData PeriOp Manager©, where a large-screen display provides the surgical team with full situational awareness of the patient and procedure, including patient allergies, medications, pathology specimens, and running status updates on blood pressure and other vital readings (Figure 2). This display synthesizes and presents the essential case information needed by clinicians, automatically aligned with case workflow. Each of these data elements must come from the EHR or ARK systems, or directly from physiological monitors or their software gateway.
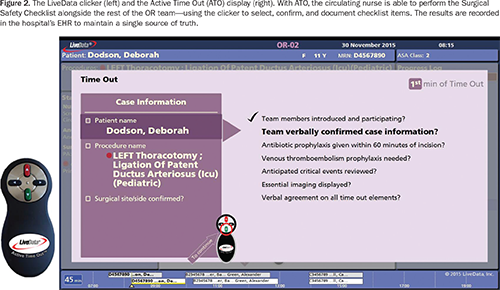
With dashboards such as these, patient safeguards mandated by CMS, The Joint Commission, and other healthcare authorities are embedded in the system, enabling clinical staff to comply with protocol activities, such as performing, documenting, and monitoring the Surgical Safety Checklist (Figure 3).
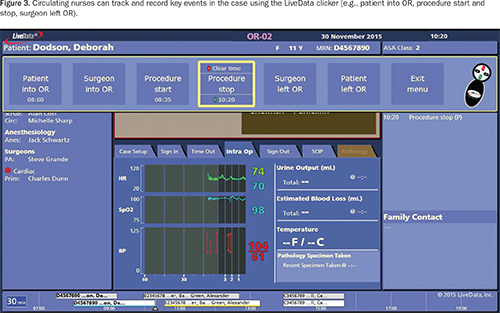
Dashboards like these also allow circulating nurses to track and record key events in the OR so that data required for metric measurement is added in real time. Examples include timestamps for case events, such as patient in and first incision; performance of compliance activities, such as the Time Out Checklist; and workflow information, such as the time taken to clean the room (see sidebar below). These events are then recorded back into the EHR.
Information sharing from various IT-enabled applications and devices within the perioperative suite can enable an integrated situational view via a set of quickly readable dashboards for clinical staff. The interoperability mechanisms employed are predominantly HL7 interfaces that provide real-time, two-way data coordination between a centralized data manager for the dashboards in the perioperative suite and the hospital EHR system, ARK system, and physiological monitoring devices, as well as real-time location systems used to track patients and assets.
Discussion
The dashboards pictured above demonstrate just one example of how interoperability can be leveraged to deliver the right information to the right people at the right time and place, and to improve the customer experience. Systems from which the dashboards pull information include commercial EHR systems, ARK systems, and a variety of other devices and interfaces, including numerous brands and models of physiological monitors, real-time location systems, and lab systems.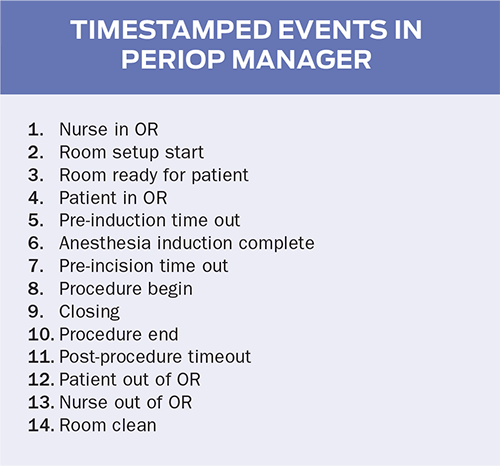
Dashboards such as LiveData PeriOp Manager have the capacity to implement interoperability using the HL7 v3 interface and have done so successfully at various hospitals. However, implementing an HL7 interface for these systems has met with political and market pressures from hospitals and vendors, requiring extra attention on the part of LiveData to ensure that all stakeholders are in agreement as to the clinical value of each interface as well as the technical details of the interface design.
Organizationally, this requires a multidimensional interaction between the hospital perioperative staff, hospital IT and biomed staff, LiveData, and occasionally the EHR and device vendors themselves. Because the product is designed to aid in information fusion for any particular hospital’s workflow, the specific requirements for HL7 interfaces may have to be configured differently for every hospital. In addition, each hospital divides critical information between the EHR and ARK systems according to its own methodology and workflow. For instance, some hospitals keep surgical consents in the ARK system as the primary record, while others keep them in the EHR. Therefore, the workflow dashboards must accommodate variations in workflow and data storage methodologies at each hospital when planning the interface design. LiveData works with the hospital’s IT staff and the other technology vendors to configure the specific HL7 interfaces as required in support of the workflow model.
The Surgical Safety Checklist provides a great example of hospital-to-hospital variation. As stated in the Implementation Manual for the World Health Organization Surgical Safety Checklist (World Alliance for Patient Safety, 2008), “Each locale is encouraged to reformat, reorder or revise the Checklist to accommodate local practice while ensuring completion of the critical safety steps in an efficient manner.” Although most hospitals base their checklists on recommended checklist items from the World Health Organization and The Joint Commission, these checklists can still vary significantly between hospitals. As a best practice, the situational awareness dashboard vendor works with the clinical staff to model the checklist used at that hospital. It is necessary to go through a discovery process to ascertain the data requirements of each checklist at each hospital, and then map this information to the ARK or EHR.
While obtaining the necessary approvals from the stakeholders required to build and test these new interfaces is not always easy, the result of the information fusion is dramatic. The design and presence of real-time data has a dramatic impact on team coordination, predictability, and process improvement. Having information visually available to anyone walking into the OR enables the entire staff to always be on the same page, creating situational awareness and consistency in performance across the team. The clinical teams have just-in-time information, so physicians and nurses can see the real-time impact of their decisions on patient care and make adjustments right away to ensure patient safety and more predictable outcomes. The data also enables the staff to see how their actions impact performance metrics such as first case on-time starts, Surgical Safety Checklist compliance, turnover times, utilization, and scheduling. Having visual, real-time data creates a significant opportunity for sustained performance improvement.
Conclusions
Because of the highly collaborative nature of the perioperative environment, coordinated team communication is key for patient safety. Shared awareness of workflow state, required assets, and patient status by all necessary staff is required at all times to promulgate patient safety. Technology tools such as the EHR or ARK system should help to provide the right information at the right time; however, clinical vocabularies and interoperability standards for the perioperative environment are in their infancy, requiring specific vendor-supplied interfaces to be created on a case-by-case basis. Identifying and extracting the right information is nontrivial because that information is located in disparate IT systems and numerous locations, depending on each hospital’s particular workflow. Interoperability between IT systems in the perioperative suite is not yet mature enough to guarantee all of the required information can be presented in a concise yet comprehensive manner that provides for “heads-up” awareness of workflow as opposed to “heads-down” recording of documentation. Reasons for lack of interoperability stem from still-evolving ontologies and standards derived from them. There is also a need for a common understanding of how closer coupling of IT systems can provide better IT to clinical users. Overcoming any additional technical risks is worth the effort.
Before interoperability comes adoption. Although the American Recovery and Reinvestment Act of 2009 has influenced a significant number of hospitals to purchase and deploy EHR and ARK systems, much work remains to learn and implement best practices for these technologies, and to determine how tying these systems together can have a multiplicative effect on patient safety and successful outcomes.
* For additional discussion of ontologies in medicine, see http://www.openclinical.org/ontologies.html
Charlie Berg is vice president of engineering at LiveData, Inc. He holds a BSEE and BA from the University of Pennsylvania and studied artificial intelligence at MIT. He can be contacted at cberg@livedata.com.
References
Ahmadian, L. (2011, January 26). Data interchange standards in healthcare: Semantic interoperability in preoperative assessment (PhD thesis). University of Amsterdam Digital Academic Repository (UvA-DARE). Retrieved from http://dare.uva.nl/record/1/366121
Ahmadian, L., Cornet, R., van Klei, W. A., & deKeizer, N. F. (2011). Data collection variation in preoperative assessment: A literature review. Computers Informatics Nursing, 29(11), 662–670. doi:10.1097/NCN.0b013e31820660bb
American Hospital Association. (2015). Why interoperability matters. Retrieved from http://www.aha.org/content/15/interoperabilitymatters.pdf
Cohen, N. H. (2015). Coordinating perioperative care: Building bridges and aligning incentives. ASA Newsletter. Retrieved from http://www.asahq.org/resources/publications/newsletter-articles/2015/september-2015/coordinating-perioperative-care
Dixon, B. E., & Zafar, A. (2009, January). Inpatient computerized provider order entry: Findings from the AHRQ Health IT Portfolio (Prepared by the AHRQ National Resource Center for Health IT). AHRQ Publication No. 09-0031-EF. Rockville, MD: Agency for Healthcare Research and Quality. Retrieved from https://healthit.ahrq.gov/ahrq-funded-projects/emerging-lessons/computerized-provider-order-entry-inpatient/inpatient-computerized-provider-order-entry-cpoe
IHE PCC Technical Committee. (2014, December 3). IHE patient care coordination (PCC) technical framework supplement. CDA content modules. Trial implementation. Retrieved from http://www.ihe.net/uploadedFiles/Documents/PCC/IHE_PCC_Suppl_CDA_Content_Modules.pdf
Ku, H.-L., Wang, P.-C., Su, M.-C., Liu, C. C. H., & Hwang, W.-Y. (2011). Application of radio-frequency identification in perioperative care. AORN Journal, 94(2), 158–172. doi:10.1016/j.aorn.2009.12.034
Lonergan, D. F., & Ehrenfeld, J. M. (2012). Advancement of information technology in outpatient and perioperative settings to support patient care and translational research. Pain Management, 2(5), 445–449. doi:10.2217/pmt.12.43
Lundberg, C. B., Warren, J. J., Brokel, J., Bulechek, G. M., Butcher, H. K., Dochterman, J. M., … Giarrizzo-Wilson, S. (2008). Selecting a standardized terminology for the electronic health record that reveals the impact of nursing on patient care. Online Journal of Nursing Informatics, 12(2). Retrieved from http://www.himss.org/ResourceLibrary/ResourceDetail.aspx?ItemNumber=10610
St. Jacques, P. J., & Minear, M. N. (2008, August). Improving perioperative patient safety through the use of information technology. In K. Henriksen, J. B. Battles, M. A. Keyes, & M. L. Grady (Series Eds.), Advances in patient safety: New directions and alternative approaches: Vol. 4 technology and medication safety. Retrieved from http://www.ahrq.gov/downloads/pub/advances2/vol4/advances-stjacques_105.pdf
Trentman, T. L., Mueller, J. T., Ruskin, K. J., Noble, B. N., & Doyle, C. A. (2011). Adoption of anesthesia information management systems by US anesthesiologists. Journal of Clinical Monitoring and Computing, 25(2), 129–135. doi:10.1007/s10877-011-9289-x
World Alliance for Patient Safety. (2008). Implementation manual for the World Health Organization Surgical Safety Checklist. First edition. Geneva, Switzerland: World Health Organziation. Retrieved from http://www.who.int/patientsafety/safesurgery/tools_resources/SSSL_Manual_finalJun08.pdf
