From Smart Pumps to Intelligent Infusion Systems – The Promise of Interoperability
By Tim Vanderveen, PharmD, MS
Infusing Patients Safely:
|
|
A little more than a decade ago the introduction of “smart” pumps with dose error-reduction systems (DERS) dramatically improved the safety of intravenous (IV) infusion therapy. Wireless connectivity enhanced system management and laid the foundation for integrating smart pumps with other systems and devices. Now, being able to integrate what previously have been isolated “islands” of individual infusion pumps with other systems opens the door to interoperability and further dramatic improvements in infusion safety, nursing and pharmacy productivity, clinical decision-making, patient monitoring, alarm notification, and reduction in variation and waste.
Interoperability is a journey and not a destination. Hospitals can start anywhere in the spectrum of opportunities that will be coming along, based on need and HIT capabilities. However a hospital chooses to begin, an ultimate goal is to connect and monitor all infusion-related systems with surveillance patterned after the air traffic control systems. In much the same way as the air traffic controller works with pilots to help planes fly more safely, one can envision a future IV medication system that is fully integrated with other systems and would automatically flag any critical, infusion-related situation that requires immediate attention, adding a new dimension to IV infusion safety.
The information in this article is drawn from more than four decades’ academic and industry involvement with improving IV infusion safety and includes descriptions of major accomplishments to date, examples of the changes happening right now, and a future vision for further advances (sidebar), some of which are already in use in early-adopter hospitals.
From “Dumb” to “Smart” Pumps
The first programmable IV infusion pumps came into use more than 40 years ago. Being able to program a specific rate and volume made modern infusion therapy possible; but these “dumb” pumps could accept any infusion rate from 0.1 to 999 mL/hr or higher. Programming 54 instead of 5.4, 800 instead of 8, or entering the volume as the rate could each deliver a fatal dose. Compared to medications delivered via other routes, IV medication errors are twice as likely to cause patient harm (Proceedings, 2008). For the next three decades, the potential for pump mis-programming and other errors remained a critical issue.
In the late 1990s a technological breakthrough—electronically erasable programmable read-only memory (EEPROM)—made it possible to develop “smart” pumps with safety software that could be customized to a hospital’s specific care areas and patient types. The customized software generated an alert or prevented infusion altogether if pump programming exceeded the hospital-established limits. The widespread implementation of such pumps significantly improved IV medication safety. In more than 10 years since their introduction, smart pumps have:
- Fostered development of drug dose limits.
- Promoted standardization of concentration and dosing units.
- Allowed hospitals to configure pumps to match applications.
- Provided a “treasure trove” of infusion data.
- Documented many “good catches” of prevented programming errors.
- Uncovered high degree of variation in infusion practices.
- Identified human factors issues/opportunities for manufacturers.
- Promoted wireless connectivity/server applications.

Figure 1. Infusion Auto-Pump Programming Using Barcode Scanning
The most significant advance in smart pump use came in 2003 with the introduction of wireless connectivity. The implementation of bidirectional wireless connectivity between hundreds of pumps and a single server allowed hospitals to upload software revisions and download infusion data much more easily. This greatly enhanced infusion safety and continuous quality improvement (CQI) efforts. A 2005 study of 426 IV infusions prior to smart pump implementation showed that 67% had one or more discrepancies and errors, including wrong infusion rates and doses, infusions without orders, and infusions continuing after discontinuation orders (Husch et al., 2005). For errors associated with pump programming, only one potentially would have been identified by DERS. A 2010 study evaluating almost 600 in-process infusions showed that 24% of drug infusions and 42% of fluid infusions had a “mismatch” between computerized prescriber order entry (CPOE) orders and smart pump programming (Russell et al., 2010). Available pumps have limitations such as the following:
- Typically not assigned to specific patients.
- Not aware of intended therapy.
- Cannot prevent drug mix-ups, incorrect library selection.
- Do not record caregiver or reason for alert overrides.
- Do not populate infusion records.
- Do not maximize value of BCMA.
- Do not overcome poor compliance with DERS use or rapid overrides of alerts.
- Do not communicate alarms, alerts, or status of infusions in near-real time.
Smart pumps are still not “smart” enough to ensure the “Five Rights” of right drug, dose, route, patient, and time, much less right response and documentation. Barcode medication administration (BCMA) can help ensure these rights and works very well for tablets, unit-dose liquids, and injections for which the drug administration is a discrete “event.” Scanning the nurse, patient, and medication and administering the drug completes the event. However, many IV infusions are a continuing “process” involving initial programming and often subsequent changes with multiple nurses involved in the therapy. While smart pumps and BCMA coexist in many hospitals, except in a very small number they are not integrated. Addressing the complexity of IV therapy requires an integrated approach (Husch et al., 2005).
From “Smart” Pumps to “Intelligent” Systems
A major limitation has been that even with connectivity, infusion pumps typically operate in insolation—not assigned to a particular patient, not aware of the intent of therapy, unaware of caregiver proximity, and unable to interact with other safety technologies. Wireless connectivity and direct communication with BCMA, the hospital information system (HIS), and other systems can overcome these shortcomings and elevate the current smart pumps to the new level of “intelligent” infusion system (Figure 1, pg. 24). Fully developing and implementing such systems will take time, but the impact will be dramatic.
Consider that infusion pump auto-programming and auto-documentation first went live December 2003 at Pittsburgh’s Ohio Valley General Hospital. Barcode scanning the IV container label triggered the transfer of programming information from the BCMA system to the pump. Infusion data were automatically sent from the pump to the electronic medication administration record (eMAR). From December 2003 to April 2004, medication errors that needed to be averted declined by 12% (Obsheatz, 2004). However, clinical scope, technologies, analytics, and expertise required further development before widespread implementation would be possible.
The 2011 American Society of Health-System Pharmacists National Survey showed that in the intervening eight years, the vast majority of hospitals had implemented or budgeted for the foundational technologies of CPOE, BCMA, smart pumps, and electronic medical records (EMRs) (Pedersen et al., 2012). Almost a decade after Ohio Valley General Hospital’s implementation, the technologies, software applications, regulatory approvals, and multidisciplinary teams were in place in most large hospitals to implement scalable, sustainable, reliable smart pump-EMR integration for house-wide clinical use.
 |
|
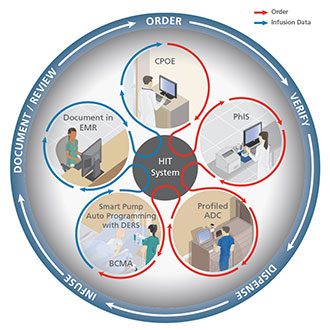
| Figure 2. Fully Integrated, Closed-Loop, Medication Safety System ©2013 CareFusion |
Possible Starting Points
Several factors make infusion pumps an ideal starting point for interoperability: the very large number of devices in a typical hospital, the critical importance of the drugs being infused, the growing base of wirelessly connected pumps already installed, and their uniquely bidirectional information transfer, both from and to the pump. A few hospitals have already implemented closed-loop systems that integrate BCMA, smart pumps, and the electronic medical record (EMR), as described below. But other entry points are also possible. For example, one hospital might decide that interfacing the smart pump and BCMA systems is the highest priority, while another might choose to work on sending alarms directly to the patient’s clinician. An ultimate goal is to connect and monitor all infusion-related systems in a type of “air traffic control” surveillance that would automatically flag any critical, infusion-related situation that requires immediate attention.
Associating Pumps and Patients
A fundamental requirement for infusion pump interoperability is the ability to associate the pump and the patient. Without this association, the vision cannot be realized, and infusion pumps, despite wireless connectivity, will continue to be islands of information. This limits their ability to be integrated with data from other systems.
The good news on that front is that today some infusion pumps can be associated with specific patients in a variety of ways, including manual entry of the patient ID using the pump key pad, using a barcode scanner integrated into the infusion pump to scan the barcode on the patient’s wristband or IV container label, or using a recently introduced patient-pump association application on the BCMA scanner, whether handheld or on a computer on wheels. An immediate benefit of this patient/pump association is that the CQI data from the smart pump DERS logs now can be put into the patient context, which makes it possible to retrospectively analyze specific DERS events such as a high-risk override or incorrectly programmed infusion. The longer-term benefits will be discussed later, as patient/pump association is an enabler for all future interoperability.
Auto-Pump Programming and Auto-Documentation
Two capabilities have been at the top of nurses’ integration wish list: the ability to automatically send the physician’s order to pre-program the infusion parameters directly into the pump, and the ability to automatically record the initial programming and all subsequent changes in the EMR, so the clinician only has to confirm the pump programming and infusion record. After many years of development and clinical testing, these capabilities now have been implemented for regular clinical use (Vanderveen, 2013). Integrating smart pumps not only with the BCMA system but also with the EMR creates a closed-loop, fully integrated medication safety system for both large-volume and syringe IV infusion pumps that accomplishes both auto-pre-programming and auto-documentation (Figure 2) (Vanderveen, 2013).
In this system, a physician orders a medication into the EMR using CPOE. A pharmacist then verifies the order to ensure appropriateness and sends it to the patient’s EMR. Prior to administration, a nurse scans the patient’s armband and the drug label to verify the right patient, medication, time, dose, and route against the order in the EMR. For infusions, one additional scan—that of a barcode on the smart pump—triggers wireless transmission of the ordered infusion parameters from the EMR to preprogram the pump. The nurse verifies the information on the smart pump, accepts the data, and the infusion begins. Throughout infusion, the DERS software in the pump acts as an additional safety feature that continues to protect against errors in manual programming of titrations, bolus doses, STAT infusions, and also infusions for which there would be no physician’s order, such as in anesthesia and procedural sedation. For the initial programming and all subsequent changes, the rate, dose, infused volume of medication, and other data are wirelessly sent back to the patient’s EMR from the smart pump for the nurse to review and accept into the EMR (Vanderveen, 2013). Nurses must confirm the correct documentation, but manual records are eliminated.
Auto-documentation provides substantial productivity gains for nurses. Especially with critically ill patients on multiple pumps, documenting their multiple infusions requires a considerable amount of time, is often delayed, and may introduce critical errors. Automatically documenting the infusion history via the wireless transfer of each patient’s infusion pump data to the EMR allows the nurse to concentrate more on patient care. Physicians, pharmacists, nurses, respiratory therapists, and other staff members benefit from having clear, accurate, and timely documentation to use in managing each patient’s therapy.
Patient Monitoring
Many IV infusion medications are high-alert drugs with a narrow therapeutic index. Careful monitoring is required to help ensure that a given dose is therapeutic and not toxic. Today there are only two examples of systems that fully integrate an infusion pump with patient monitors: one for administering and monitoring minimal-to-moderate sedation and a second for administering and monitoring patients receiving patient controlled analgesia (PCA). For example, the patient response to opioids delivered via PCA is highly variable, and patients at high risk of opioid-induced respiratory depression are not easily identified. Typically, patients receiving PCA therapy are monitored by intermittent clinician assessment, but during the first 24 hours and at night, clinicians may not monitor a patient frequently enough and over-medication may go undetected. Integration of the PCA pump with pulse oximetry and capnography (Figure 3) with automatic PCA pump pause (with alarm), if oxygen level and/or respiratory rate drop to potentially dangerous levels, has added a much needed safety net for PCA patients typically cared for in medical/surgical units. In the future, interoperability may be used to connect separate devices and systems to perform similar monitoring of a patient’s blood pressure, blood glucose, or other response to infusion.
 |
|
| Figure 3. PCA Pump Integrated with Pulse Oximetry and Capnography |
Infusion Status Monitoring
In the early 1970s, responsibility for preparing IV infusion admixtures began to shift from the physicians and nurses to the hospital pharmacy. This shift has brought numerous advantages with regard to safety, sterility, accuracy, compatibility, and labeling, but without knowing the status of each patient’s infusions, scheduling subsequent IV infusions remains problematic. Infusions may be prepared and not used, other infusions may not be ready on time, etc. Wireless connectivity can change this. Knowing which pumps are assigned to which patients and the status of each patient’s infusions will allow pharmacy to improve workflow, productivity, costs, and nursing-pharmacy relations. The ongoing critical drug shortages, ever-increasing cost of medications, and impact of regulations on IV compounding practices are all reasons to improve communication between the bedside and the compounding pharmacy. Near-real time infusion status on a pharmacy dashboard can alert the pharmacy staff to infusions that have been discontinued, infusion rates that have changed, and infusions that were ordered but never started.
Pump Maintenance
Maintaining hundreds and, in some hospitals, more than 1,000 infusion pumps in good working order is a huge task. Although modern infusion pumps have maintenance logs, a biomedical department often receives a pump with only a label attached that indicates “broken.” Adverse patient events are frequently attributed to pumps that were not removed from service despite having performance issues. An example is a battery that no longer holds a charge. Despite frequent “low battery” alarms and needing to be charged for long periods, the pump may remain in clinical use. If the battery suddenly dies during a transport or there is a power interruption and a critical infusion stops, the adverse effects on the patient could be severe. Additionally, some performance issues are invisible to the clinicians but may appear in the log during routine maintenance.
Similar to the pharmacy dashboard, an integrated dashboard in the biomedical department could display the operating parameters for each pump, identify issues, and provide a pump’s location, so that pump issues can be identified and addressed in a timely manner, before an adverse event occurs. The direct link between each pump and the biomedical department would be similar to the automotive industry’s use of in-vehicle diagnostics and communication systems.
Alarm Management
Publication of The Joint Commission’s Sentinel Event Alert, Issue 50, “Medical Device Alarm Safety in Hospitals” (2013 April 8), and National Patient Safety Goal 06.01.01, “Improve the safety of clinical alarm systems” (2013), has focused hospitals’ attention on ways to reduce alarms, make patient care areas quieter, and increase patient and family member satisfaction. In a typical hospital, hundreds of infusion pumps sound alarms and alerts 24 hours per day. Adding to the noise level are U.S. and international standards that must be met regarding alarm loudness. Most alarms require a bedside visit to silence the alarm and determine the cause. Outside of the ICU, however, many pump alarms are not critical and may not require immediate attention.
The combination of patient-pump association and knowing the patient location, drug or fluid being infused, type of alarm, and the clinician responsible for the patient are the ingredients needed to address this issue effectively. Alarm-management companies are developing systems to distribute pump alerts and alarms directly to the patient’s caregiver, potentially in advance of the actual bedside alarm. For example, sending a message to the patient’s nurse that an infusion container has 15 minutes before an “infusion complete” alarm sounds could eliminate the bedside alarm all together. Smart alarms and intelligent alarms systems are exciting opportunities for improving safety, increasing nursing productivity, and increasing patient and family member satisfaction.
 |
|
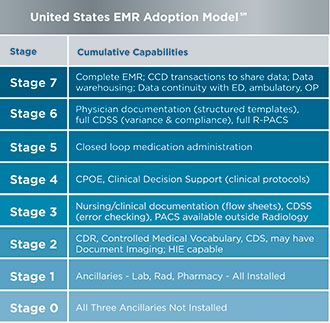
| Figure 4. U.S. Electronic Medical Record Adoption Model |
“Air Traffic Control” Integrated Surveillance
It’s important to bear in mind that interoperability is a journey, not a destination. Even with interoperability, a system doesn’t necessarily flag things that need to be brought to someone’s attention. The next huge step forward will be systems that can act as a type of “air traffic controller” that knows whom to contact and can send an alert and/or command directly to the appropriate “pilot,” concentrating on 747s and 737s, not Piper Cubs.
In the future, once the pump is assigned to the patient, a complete list of all active orders will be easily accessed. The smart pump can send information on everything the pump is doing to the server. A pharmacist, nurse, or physician can instantly see if an infusion is on- or off-target, as the intelligent surveillance system automatically flags situations such as the following:
- The infusion that is running is not what was ordered; for example, the order is for heparin 1000 Units/hr, but the pump is programmed for 100 Units/hr.
- A nurse has overridden an alert, potentially leading to a serious adverse event.
- A drug infusion has been ordered, but there is no evidence in the system that the drug is being infused.
- An order has been discontinued, but the infusion continues.
- A patient has been on an IV anticoagulant, but the required clotting studies have not been ordered.
- The patient’s potassium level is low, and the nurse should not administer the next dose.
In much the same way that alerts need to be managed to avoid fatigue and help staff to recognize the critical alerts, intelligent systems will need to provide enterprise-wide surveillance that automatically flags issues that require immediate attention and clinical decision support systems to help guide the appropriate response.
Making the Journey
For many hospitals, interoperability through integrated systems is still a long way off. But even with today’s stand-alone devices, hospitals can do much to optimize use of their existing smart pumps and prepare for the implementation of integrated systems. For example, hospitals can:
- Ensure that all smart pumps are on wireless networks to optimize smart pump drug library management.
- Make sure that all available safety features are enabled.
- Manage the drug libraries aggressively so they reflect best practice and are easy for nurses to use.
- Make sure that important alerts are not masked by nuisance alerts.
- Regularly analyze data on alerts and subsequent actions to provide actionable information that can be used to help improve therapy, medication safety, and clinical alarm management.
- Track and report CQI and compliance data to help achieve high rates of compliance with use of smart pump safety features.
- Take the necessary steps to advance from HIMSS’s EMR Adoption Stages 1 to 5 (Figure 4), in order to prepare for more advanced integration.
The purpose of making this journey, of course, is not just to achieve ever-increasing technological integration and interoperability but to improve IV infusion safety, quality of care, clinician satisfaction, financial performance, and patients’ well-being. Developing and holding the vision of interoperability that is best suited to one’s own institution is a critical first step.
Tim Vanderveen is vice president of the CareFusion Center for Safety and Clinical Excellence in San Diego, California. He may be contacted at tim.vanderveen@carefusion.com.
References
Healthcare Information and Management Systems Society. US EMR Adoption Model(SM). Retrieved April 18, 2014 from http://www.himssanalytics.org/hc_providers/emr_adoption.asp
Husch, M., Sullivan, C., Rooney, D., Barnard, C., Fotis, M., Clarke, J., & Noskin, G. (2005). Insights from the sharp end of intravenous medication errors: Implications for infusion pump technology. Quality and Safety in Health Care, 14(2), 80-86. doi:10.1136/qshc.2004.011957
The Joint Commission. (2013, April 8). Medical device alarm safety in hospitals. Sentinel Event Alert, 50. Retrieved from http://www.jointcommission.org/assets/1/18/SEA_50_alarms_4_5_13_FINAL1.PDF
The Joint Commission. (2013). National Patient Safety Goals Effective January 1, 2014. Hospital accreditation program. Retrieved from http://www.jointcommission.org/assets/1/6/HAP_NPSG_Chapter_2014.pdf
Obsheatz, M. (2004). Integrating bar code medication administration and intravenous medication safety systems. In: P. J. Schneider (Ed.). Measuring medication safety with smart IV systems. HealthLeaders, 7(12suppl), 51-55.
Pedersen, C. A., Schneider, P. J., & Scheckelhoff, D. J. (2012). ASHP national survey of pharmacy practice in hospital settings: Dispensing and administration—2011. American Journal of Health-System Pharmacists, 69(9), 768-785.
Proceedings of a summit on preventing patient harm and death from IV medication errors. (2008). American Journal of Health System Pharmacists, 65, 2367-2379.
Russell, R. A., Murkowski, K., & Scanlon, M.C. (2010). Discrepancies between medication orders and infusion pump programming in a paediatric intensive care unit. Quality and Safety in Health Care, 19(Suppl3), i31-5. doi:10.1136/qshc.2009.036384
Vanderveen, T. (2013). Intravenous infusion medication safety: The vision becomes reality. Patient Safety & Quality Healthcare, 10(2), 24–30. Retrieved from http://www.psqh.com/marchapril-2013/1598-intravenous-infusion-medication-safety-the-vision-becomes-reality.htmlfusing Patients Safely: A Future Vision
